When you pick up a prescription, you might not realize that the drug you’re getting isn’t always the one your doctor originally wrote. In many states, pharmacists are allowed to swap out brand-name drugs for generics without asking you first. This isn’t random-it’s the result of deliberate state policies designed to save money on prescription drugs. And it’s working. Across the U.S., states have built a patchwork of rules, financial nudges, and legal requirements to push doctors, pharmacists, and patients toward cheaper generic medications. The goal? Lower costs without lowering care.
How States Save Money Without Sacrificing Care
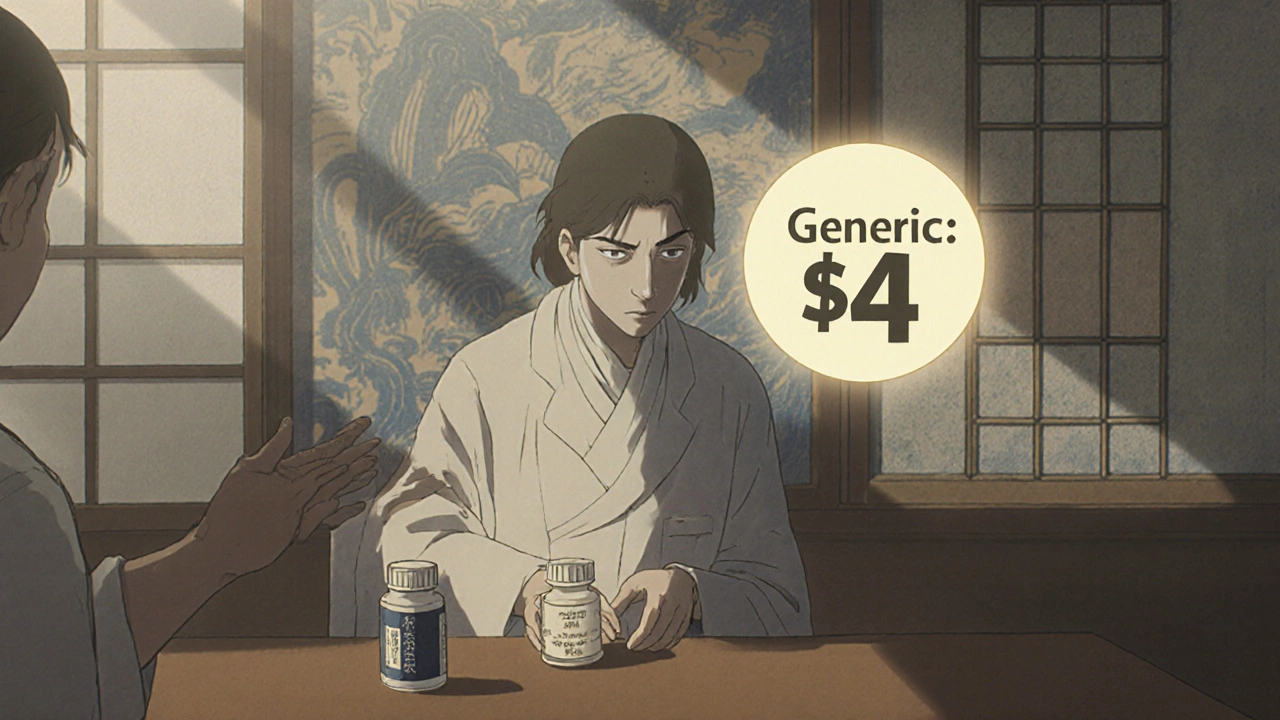
Generic drugs aren’t cheaper because they’re worse. They’re cheaper because they don’t need expensive clinical trials. Once a brand-name drug’s patent expires, other companies can make the same medicine using the same active ingredients. The FDA requires generics to be just as safe and effective. So why do brand-name drugs still dominate prescriptions? Price. A 30-day supply of a brand-name blood pressure pill might cost $120. The generic? $4.
States stepped in because Medicaid and other public health programs were spending billions on brand-name drugs that had generic alternatives. In 2019, 46 out of 50 states had a Preferred Drug List (PDL) for Medicaid prescriptions. These lists tell doctors and pharmacists which drugs are the most cost-effective. If a doctor prescribes a drug not on the list, the pharmacy might refuse to fill it-or the patient pays more out of pocket.
It’s not just about blocking brand drugs. States also reward pharmacies and patients for choosing generics. Some states pay pharmacists a higher fee to dispense a generic. Others require patients to pay a $10 copay for a brand drug but only $5 for the generic. That small difference changes behavior. People are more likely to pick up their meds if they cost less. And pharmacies? They’re incentivized to swap out the expensive version-even if the doctor didn’t ask for it.
The Power of Presumed Consent
One of the most effective tools states use is called presumed consent. This means pharmacists can automatically substitute a generic drug unless the doctor writes “dispense as written” or the patient says no. It’s the opposite of explicit consent, where the patient must give permission before the swap happens.
A 2018 study from the National Institutes of Health found that states with presumed consent laws saw a 3.2 percentage point increase in generic dispensing compared to states that required patient permission. That might sound small, but multiply that across millions of prescriptions, and you’re talking about billions in savings. The study estimated that if all 39 states with explicit consent laws switched to presumed consent, they could save $51 billion a year.
Why does this work so well? Because it removes friction. Most patients don’t care if they get the generic. They just want the medicine to work. But if you have to ask them every time, they might forget, get confused, or say no out of habit. Presumed consent makes the smart choice the easy choice.
Why Mandatory Substitution Doesn’t Work
Some states tried forcing pharmacists to substitute generics no matter what. But research shows those rules barely moved the needle. Why? Pharmacists were already substituting generics anyway-they made more money on them. The profit margin on a generic drug can be 10 times higher than on a brand-name one. So even without a law, pharmacists had a strong reason to swap.
What really changes behavior isn’t forcing the pharmacist. It’s changing what the patient pays. When a patient sees a $20 copay for a brand drug and a $5 copay for the generic, they choose the cheaper option. That’s why states are moving away from top-down mandates and toward patient-facing incentives. The real leverage isn’t in the pharmacy counter-it’s in the wallet.
Medicaid’s Hidden Engine: The Rebate System
Behind every generic drug on a state’s Preferred Drug List is a complex financial deal called the Medicaid Drug Rebate Program. Since 1990, federal law has required drugmakers to pay rebates to states for every prescription filled through Medicaid. For generics, the minimum rebate is 13% of the drug’s average price. But states don’t stop there. Forty-six states in 2019 negotiated extra rebates on top of that-sometimes doubling or tripling the savings.
These rebates are why states can afford to make generics the default. The more generics they use, the more money they get back from drug companies. It’s a self-reinforcing loop: lower prices → higher use → bigger rebates → more savings. That’s why states like California and New York have some of the most aggressive generic substitution policies-they’re not just trying to cut costs, they’re building a financial system that rewards cheaper drugs.
But there’s a catch. Sometimes, generic manufacturers face unexpected rebate increases that make their drugs unprofitable. If a generic drug’s price stays the same but Medicaid’s rebate formula changes, the manufacturer might lose money on every pill sold. That’s led to shortages in some cases, where a generic disappears from shelves because no one wants to make it anymore. States are learning this the hard way-pushing too hard on price can break the supply chain.
340B and the Safety-Net Puzzle
Another layer of the puzzle is the 340B Drug Pricing Program. Created in 1992, it lets hospitals and clinics that serve low-income patients buy drugs at steep discounts-often 20% to 50% off. These are safety-net providers: community health centers, rural hospitals, free clinics. They rely on 340B to stretch their budgets.
But here’s the twist: states have to reimburse these providers for Medicaid prescriptions based on what they actually paid (called Actual Acquisition Cost), not a fixed rate. After a 2016 federal rule, states had to align their payments with 340B prices. That meant some states had to pay pharmacies less for brand-name drugs, which pushed providers even harder toward generics. It wasn’t a policy change-it was a financial domino effect.
For patients at these clinics, it means more access to affordable meds. For states, it means tighter control over how drug money flows. But it also creates tension. If a pharmacy’s reimbursement drops too low, they might stop carrying certain generics. Or worse-they might stop serving 340B patients altogether.
What’s Next? The Drug List
At the federal level, the Centers for Medicare & Medicaid Services (CMS) is testing a new idea: the $2 Drug List. It’s simple-any generic drug that costs $2 or less per 30-day supply gets a flat copay of $2, no matter what. No prior authorization. No complex formularies. Just an easy, predictable price.
This isn’t mandatory for states, but it’s a blueprint. If it works for Medicare Part D beneficiaries, states might copy it for Medicaid. The idea is to cut through the noise. Patients don’t need to understand formularies or rebates. They just need to know: “This pill is $2. That one’s $40. Pick the $2 one.”
It’s a shift from complex regulation to simple clarity. And it might be the future. States are realizing that the best way to get people to choose generics isn’t to punish them for choosing brands-it’s to make the generic option so easy and affordable that it’s the only choice that makes sense.
The Big Picture: Savings, Risks, and Real People
States have saved hundreds of billions by pushing generics. But it’s not all smooth sailing. Drug shortages, rebate surprises, and manufacturer pullouts are real risks. And while most patients don’t mind generics, some worry they’re “second-rate.” That’s where education matters. A patient who understands that the generic for their asthma inhaler is identical in effectiveness is more likely to stick with it.
The real success of these policies isn’t in the numbers-it’s in access. A diabetic in rural Ohio can afford insulin because the state made the generic version the default. A veteran in Michigan gets his blood pressure pills without skipping doses because his copay is $5, not $50. That’s what these laws are really about: making sure people get the medicine they need, without going broke.
There’s no perfect system. But the trend is clear: the future of drug pricing isn’t about controlling doctors. It’s about designing systems where the cheapest, safest option is also the easiest one to choose.
Are generic drugs really as good as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, purity, and effectiveness. The only differences are in inactive ingredients (like fillers or dyes) and packaging. For over 90% of prescriptions, generics work just as well-and cost a fraction of the price.
Can my pharmacist switch my brand-name drug without telling me?
In 31 states with presumed consent laws, yes-pharmacists can substitute a generic without asking you, unless the doctor specifically wrote "dispense as written" on the prescription. In the other 19 states, pharmacists must get your permission first. Always check your receipt or ask the pharmacist if you’re unsure what you received.
Why do some generic drugs cost more than others?
Even among generics, prices vary. That’s because multiple companies can make the same drug, and competition drives prices down. But if only one company makes a generic, or if there’s a shortage, the price can spike. Some states use Maximum Allowable Cost (MAC) lists to cap how much they’ll pay for a generic, which helps keep prices stable.
Do generic prescribing laws hurt drug innovation?
No. Generic laws target drugs whose patents have already expired. They don’t affect new drugs still under patent protection. In fact, by lowering overall drug spending, they free up money for other healthcare needs. The real pressure on innovation comes from high prices on new brand-name drugs-not from the use of older generics.
What happens if a generic drug I rely on disappears?
If a generic is pulled from the market due to shortages or unprofitability, your pharmacy will notify you and your doctor. You may need to switch to another generic version or, in rare cases, go back to the brand-name drug. Some states track drug availability closely and work with manufacturers to prevent shortages. If you’re concerned, ask your pharmacist to alert you if your medication changes.
Robert Merril
November 17, 2025 AT 12:14So let me get this right the government pays pharmacists extra to give me a pill that works the same but costs 10x less and somehow this is controversial
People are gonna freak out because they think generics are made in a basement by dudes named Boris but the FDA says its the same damn thing
Also why are we still paying 120 for blood pressure meds when the generic is 4 i dont even know anymore
Georgia Green
November 19, 2025 AT 03:01Just a heads up i had a generic for my thyroid med last year and it made me feel awful turns out the filler was different and my body reacted
Not saying all generics are bad but dont assume theyre all identical
Ask your pharmacist for the manufacturer code if you notice a change in how you feel
Julie Roe
November 20, 2025 AT 02:17I love how this post breaks down the real mechanics behind drug pricing instead of just screaming about corporate greed
Most people dont realize that the real leverage isnt in forcing pharmacists to swap drugs its in making the patient feel like theyre getting a better deal
That $5 vs $20 copay difference is a psychological game changer
And the Medicaid rebate system is genius really its like a tax incentive for doing the right thing
Its not about controlling doctors its about making the smart choice the easy choice
And honestly if you can save billions without compromising care why wouldnt you do it
People worry about shortages but thats usually because the price is too low for manufacturers to make money not because the system is broken
We need more of these smart nudges not more mandates
Also the $2 drug list idea is brilliant simple clean and patient centered
Imagine if every prescription was like this no confusing formularies no prior auth just pick the one that costs two bucks
Thats healthcare we can actually understand
Roberta Colombin
November 20, 2025 AT 10:39As someone who works with rural clinics i can tell you the 340B program is a lifeline
Without it many of our patients would choose between food and medicine
But when states cut reimbursement too low pharmacies start dropping out
Its not about profit its about survival
We need policies that support access not just cost savings
Generics are great but only if theyre available
And if a patient cant get their medication because the pharmacy stopped stocking it because the reimbursement is too low then weve lost the point
Christina Abellar
November 21, 2025 AT 20:22My pharmacist swapped my generic without telling me and i didnt even notice
Works fine
Jennifer Howard
November 22, 2025 AT 13:58While the premise of this article is superficially compelling it fundamentally misrepresents the ethical and legal implications of presumed consent in pharmaceutical substitution
One cannot ethically assume consent for a medical intervention even when the clinical outcome is statistically equivalent
The FDA equivalence standard is a legal fiction designed to facilitate corporate profit under the guise of public health
Patients have a fundamental right to autonomy over their pharmacological regimen and the substitution of a branded medication with a generic constitutes a material change in treatment protocol regardless of bioequivalence
Furthermore the rebate system creates perverse incentives that distort the market and ultimately reduce innovation in the long term
The notion that patients do not care is patronizing and reflects a profound misunderstanding of medical agency
One must not confuse cost efficiency with ethical governance
The slippery slope of presumed consent leads inevitably to paternalistic healthcare systems where individual rights are subordinated to fiscal targets
This is not progress it is the commodification of human health
Dave Feland
November 22, 2025 AT 19:50Did you know that the FDA allows generics to vary by up to 20 in bioavailability
That means your generic blood pressure pill could be 20 weaker or stronger than the brand
And the rebate system is just a front for Big Pharma to control the market through monopolies on inactive ingredients
They make the generic cheaper to produce but add a weird filler that causes long term kidney damage
And the $2 drug list
That’s just the first step before they start putting tracking chips in the pills
Next thing you know your insulin is being monitored by the CDC
And they’ll tell you when to take it
They’ve been doing this since the 1970s
They want you dependent on the system
They dont want you healthy they want you compliant
Ashley Unknown
November 22, 2025 AT 22:43Okay so let me get this straight
Theyre swapping my meds without telling me
And then theyre paying pharmacists to do it
And the government is getting rebates from drug companies
And now theyre thinking about a $2 drug list
But wait
What if the generic is made in China
What if the active ingredient is the same but the filler is laced with something
What if the pharmacist is just a pawn in a bigger scheme
What if the whole thing is a cover for pharmaceutical corporations to dump old stock
What if my thyroid meds are actually causing my anxiety
What if the FDA is in on it
What if this is how they control the population
And what if the $2 drug list is just the beginning
And what if next they make all prescriptions mandatory
And what if they start printing the pills with barcodes that link to your social security number
And what if they track your compliance
And what if they cut your benefits if you dont take the generic
And what if this is all part of the New World Order
And what if my pharmacist knows but wont tell me
And what if I’m the only one who sees it
And what if I’m not crazy
And what if I’m the only one who cares
Jennie Zhu
November 24, 2025 AT 09:24The structural economics underpinning state-level generic substitution policies are predicated upon a confluence of regulatory arbitrage and fiscal externalization
The Medicaid Drug Rebate Program functions as a de facto price ceiling mechanism wherein manufacturers are compelled to subsidize public expenditures through mandatory rebate structures
When coupled with Maximum Allowable Cost (MAC) formularies and presumed consent statutes, these mechanisms create a non-linear incentive architecture wherein pharmacy reimbursement dynamics override prescriber autonomy
Notably, the 340B program introduces a parallel layer of price suppression that further distorts market equilibrium for safety-net providers
While the empirical outcomes demonstrate significant cost containment, the unintended consequences include therapeutic substitution-induced adverse events, supply chain fragility due to margin compression, and erosion of patient trust through procedural opacity
Moreover, the absence of robust pharmacovigilance protocols for generic-specific adverse reactions constitutes a latent public health vulnerability
Policy design must therefore evolve beyond cost-efficiency metrics to incorporate patient-reported outcomes, manufacturer accountability, and dynamic formulary monitoring
The $2 Drug List, while administratively elegant, risks exacerbating the very supply chain vulnerabilities it seeks to mitigate through homogenization of pricing incentives
True innovation lies not in simplification but in calibrated, evidence-based governance
Kathy Grant
November 26, 2025 AT 06:32I read this and I felt this deep quiet relief
Not because I’m some policy wonk but because I’ve seen what happens when people can’t afford their meds
I watched my neighbor skip her insulin doses because the brand was $400 and she was working two jobs
She didn’t know the generic was the same
She just knew she couldn’t pay
And then one day she got a call from the clinic saying they could switch her
She cried
Not because she was happy about the generic
But because she could breathe again
That’s what this is about
Not rebates or formularies or even the FDA
It’s about someone getting to live
Yes there are risks
Yes sometimes generics disappear
But the alternative is worse
People dying because they can’t afford to live
So yeah let’s fix the shortages
Let’s make sure manufacturers aren’t losing money
But let’s not throw out the system because it’s not perfect
It’s saving lives
And that’s worth fighting for
Noel Molina Mattinez
November 27, 2025 AT 07:13Pharmacists are swapping meds without telling you and you dont even notice
That’s the point
Theyre not supposed to tell you
Theyre supposed to make the swap
And youre supposed to be grateful
And if you complain theyll say you dont understand the system
But you know what
Theyre not swapping your meds
Theyre swapping your rights
And no one is talking about it
Not even the doctors
Theyre all in on it
And you just keep taking your pills
And never asking why
And that’s the real problem