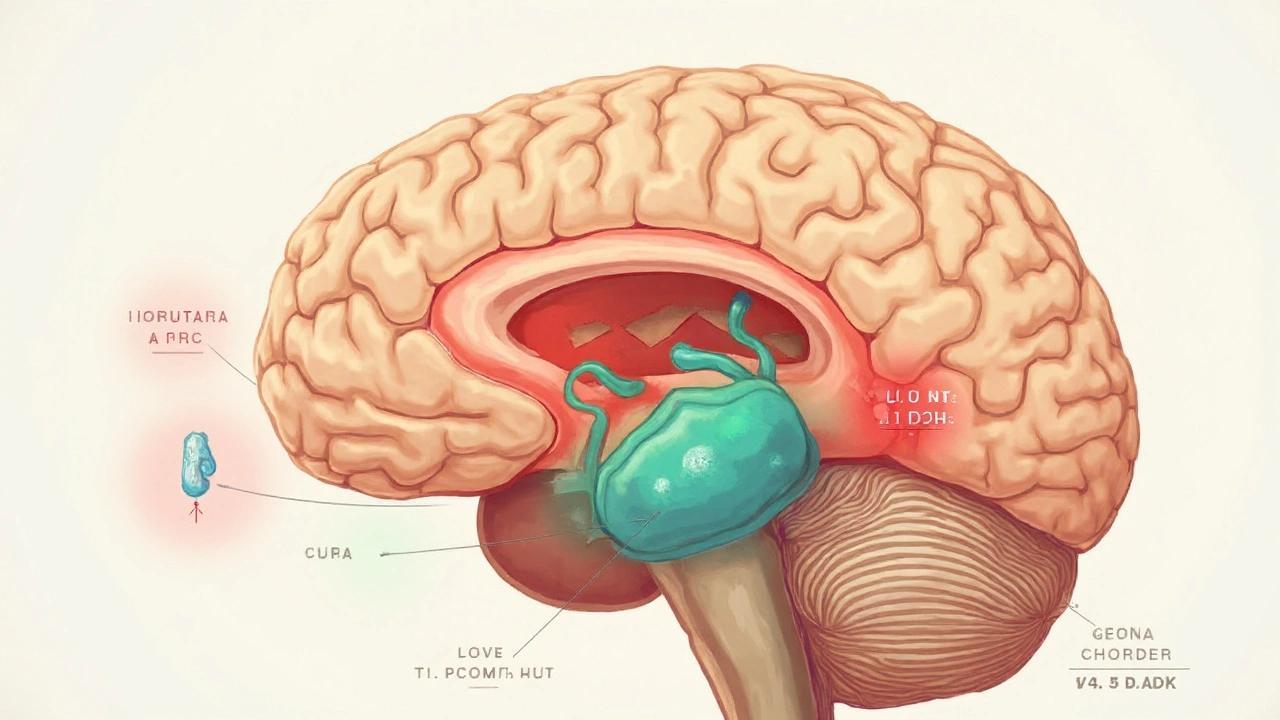
Pituitary gland disorder is a medical condition that impairs the normal function of the pituitary gland, a pea‑sized organ at the base of the brain that regulates growth, metabolism, and reproduction by releasing hormones into the bloodstream. When these hormones falter, the downstream impact on the hypothalamic‑pituitary‑gonadal (HPG) axis the hormonal circuit linking the hypothalamus, pituitary gland, and gonads can produce secondary hypogonadism, a state where the gonads themselves are healthy, but the body fails to signal them correctly.
Why the Pituitary Matters for Sexual Hormones
The pituitary secretes two key gonadotropins: luteinising hormone (LH) and follicle‑stimulating hormone (FSH). LH stimulates testosterone production in men and ovulation in women, while FSH supports sperm maturation and ovarian follicle growth. Any disruption-whether excess prolactin, reduced LH/FSH output, or structural damage-breaks the chain, leading to low testosterone or estrogen despite an intact testis or ovary.
Common Pituitary Disorders That Cause Secondary Hypogonadism
| Disorder | Primary Hormonal Effect | Typical Symptoms | First‑line Treatment |
|---|---|---|---|
| Prolactinoma a benign tumor that overproduces prolactin | Elevated prolactin suppresses GnRH → low LH/FSH | Infertility, galactorrhoea, decreased libido | Dopamine agonists (cabergoline, bromocriptine) |
| Non‑functioning pituitary adenoma tumor that compresses normal pituitary tissue | Reduced secretion of LH, FSH, and other pituitary hormones | Headache, visual field loss, fatigue, low sex hormones | Surgical resection ± hormone replacement |
| Sheehan's syndrome post‑partum pituitary infarction due to severe blood loss | Global pituitary insufficiency, especially LH/FSH | Failure to lactate, amenorrhea, chronic tiredness | Hormone replacement (thyroid, cortisol, sex steroids) |
| Empty sella syndrome flattened pituitary within the sella turcica | Variable hormone deficiencies; often mild LH/FSH drop | Headaches, occasional hormonal fatigue | Observation or targeted hormone therapy |
These four entities cover the majority of cases where a pituitary problem translates into secondary hypogonadism. Each has a distinct pathophysiology, yet they converge on the same hormonal bottleneck.
Diagnostic Roadmap: From Symptoms to Hormone Panels
When a patient presents with low libido, erectile dysfunction, menstrual irregularities, or unexplained infertility, clinicians first rule out primary gonadal failure (testicular or ovarian disease). If sperm counts, ovarian reserves, and direct gonadal imaging are normal, the focus shifts upstream.
- Serum prolactin measures the hormone that can inhibit GnRH - values >20ng/mL often hint at a prolactinoma.
- LH and FSH gonadotropins released by the pituitary - low or inappropriately normal levels in the presence of low testosterone/estradiol signal secondary hypogonadism.
- MRI of the sellar region high‑resolution imaging to spot adenomas or structural defects - the gold standard for visualising pituitary anatomy.
- Additional pituitary axes (TSH, ACTH, GH) are checked to gauge whether the disorder is isolated or part of broader hypopituitarism.
These tests together build a hormonal fingerprint that helps clinicians differentiate, for example, a prolactinoma from a non‑functioning adenoma.
Treatment Strategies Tailored to the Underlying Disorder
Because the root cause varies, treatment is never one‑size‑fits‑all. Below is a quick guide linking each disorder to its main therapeutic path.
- Prolactinoma - Dopamine agonists (cabergoline, bromocriptine) shrink the tumor and lower prolactin, often normalising LH/FSH within weeks. Surgery is reserved for resistant cases.
- Non‑functioning adenoma - Transsphenoidal surgery removes the mass, relieving compression on normal pituitary cells. Post‑op hormone replacement may be needed if LH/FSH remain low.
- Sheehan's syndrome - Immediate hormone replacement for cortisol, thyroid, and sex steroids is lifesaving. Over time, doses are adjusted based on blood tests.
- Empty sella syndrome - Often observation; if LH/FSH deficiency becomes symptomatic, low‑dose testosterone or estradiol therapy can restore function.
Across all scenarios, once hormonal levels are stabilised, patients usually see improvements in libido, energy, and muscle mass within three to six months.
Monitoring and Long‑term Follow‑up
Even after successful treatment, pituitary disorders can recur or evolve. A practical follow‑up schedule looks like this:
- First 3months: check serum prolactin, LH, FSH, testosterone/estradiol every 4-6weeks.
- 6‑12months: annual MRI if a tumor was present, plus yearly full hormone panel.
- Beyond 1year: symptom‑driven labs; most patients need only a check‑in if they feel well.
Patients on hormone replacement should have bone density scans every 2-3years, as low sex steroids can accelerate osteoporosis.
Related Concepts and Next Steps for Readers
Understanding pituitary‑driven secondary hypogonadism opens the door to adjacent topics you might explore next:
- Primary hypogonadism a condition where the gonads themselves fail to produce hormones - how it differs diagnostically.
- Male infertility work‑up the full panel of tests beyond hormonal assessment - sperm analysis, genetic screening.
- Dopamine agonist side effects management of nausea, orthostatic hypotension, and impulse control issues - what patients should watch for.
- Transsphenoidal surgery minimally invasive approach to pituitary tumors - recovery timeline and risks.
These topics fit neatly into the broader knowledge cluster of endocrine health and reproductive medicine.

Frequently Asked Questions
Can a pituitary tumor cause low testosterone even if the testes are normal?
Yes. Tumors like prolactinomas raise prolactin, which suppresses GnRH release from the hypothalamus. Without GnRH, the pituitary drops LH and FSH, and the testes receive little stimulation, leading to low testosterone despite being structurally healthy.
What’s the difference between primary and secondary hypogonadism?
Primary hypogonadism originates in the gonads themselves (testes or ovaries) and shows high LH/FSH with low sex hormones. Secondary hypogonadism stems from the brain’s control centres-hypothalamus or pituitary-so LH/FSH are low or inappropriately normal alongside low testosterone or estradiol.
How quickly does medication lower prolactin levels in prolactinoma?
Dopamine agonists can halve prolactin concentrations within 1-2weeks. Most patients achieve normal levels by 6-8weeks, and tumor shrinkage often follows within 3-6months.
Is surgery ever needed for a prolactinoma?
Surgery is a last‑resort option, reserved for patients who cannot tolerate dopamine agonists or whose tumors are resistant and continue to grow despite medication.
Can hormone replacement restore fertility after pituitary damage?
Yes. Once LH and FSH levels are normalised-either through tumor treatment or direct gonadotropin therapy-spermatogenesis or ovulation can resume in many patients, though success rates vary with age and underlying damage.
What lifestyle changes help alongside medical treatment?
Weight loss, regular resistance training, adequate sleep, and limiting alcohol all improve endogenous testosterone production and can enhance the response to hormonal therapy.

Chantel Totten
September 22, 2025 AT 22:48This is one of the clearest explanations I've seen on secondary hypogonadism. I've been dealing with low testosterone for years and never realized it could be pituitary-related until my endocrinologist mentioned prolactinoma. The table comparing disorders was especially helpful - I wish more doctors broke it down this simply.
Guy Knudsen
September 23, 2025 AT 23:37Interesting how everyone treats this like it's some new discovery but the pituitary-gonadal axis has been textbook stuff since the 80s. Honestly most of these cases are just misdiagnosed low T from obesity or stress. MRI? Please. I've seen 3 guys get surgery for "adenomas" that were just ghost shadows on the scan. Real medicine doesn't need fancy imaging when you've got a good history and a basic lab panel.
Terrie Doty
September 24, 2025 AT 01:53I grew up in a household where my mom had Sheehan’s syndrome after a postpartum hemorrhage in 1987 - back when they didn’t even have cabergoline available. She was on lifelong hormone replacement, and I remember how she’d wake up every morning with a ritual of pills: thyroid, cortisol, estrogen. It wasn’t just medical - it was emotional. She lost her sense of self for years until the right doctor finally adjusted her doses. This article nails the clinical side, but I hope people remember there’s a human behind every hormone panel. The fatigue, the mood swings, the shame of not being able to lactate - it’s not just numbers. It’s identity.
George Ramos
September 25, 2025 AT 23:14Oh wow so now we're just gonna hand out dopamine agonists like candy? Cabergoline is literally a psychiatric drug repurposed to fix a "tumor" that may not even exist. The pharmaceutical industry has been pushing this narrative for decades - low T? Must be prolactinoma. Headache? Must be adenoma. They want you hooked on lifelong meds so you keep coming back for more scans and refills. And don't get me started on the MRI industrial complex - one scan costs more than my rent. Wake up people. The pituitary isn't broken - your lifestyle is. Stop letting Big Pharma sell you a brain tumor when you just need to sleep more and lift heavier.
Barney Rix
September 27, 2025 AT 14:35While the clinical overview is methodical and largely accurate, the omission of differential diagnostic criteria for hypopituitarism versus functional hypothalamic suppression is concerning. The reliance on serum prolactin as a primary screening tool is statistically unsound in populations with chronic stress or medication-induced hyperprolactinemia. Furthermore, the assertion that "most patients see improvements in libido and muscle mass within three to six months" lacks stratification by age, BMI, or baseline gonadotropin levels - rendering it clinically imprecise. A more rigorous approach would incorporate dynamic testing such as the GHRH-arginine stimulation test or hCG challenge prior to initiating replacement therapy.
juliephone bee
September 28, 2025 AT 10:51wait so if prolactin is high and testoseterone is low but testes are fine… its the pituitary? i think i read that right but i keep mixing up primary vs secondary… can someone dumb it down? like… if my body is making the right signals but the gonads arent responding thats primary? and if the signals never get sent its secondary? sorry im not med student just trying to understand my own labs