Imagine looking in the mirror and seeing everything slightly blurred, even with your glasses on. Lights glare too brightly. Reading becomes a chore. You’ve tried new prescriptions, but nothing seems to stick. If you’re in your teens or twenties and this sounds familiar, you might be dealing with keratoconus-a condition where your cornea, the clear front surface of your eye, slowly thins and bulges outward into a cone shape. It’s not rare. About 1 in 2,000 people have it. And for most, rigid contact lenses aren’t just an option-they’re the key to seeing clearly again.
What Actually Happens in Keratoconus?
Your cornea isn’t supposed to change shape. It’s meant to be smooth and dome-like, bending light perfectly onto the retina. In keratoconus, that structure breaks down. Enzymes in the cornea start breaking down collagen fibers faster than the body can repair them. The result? The center of the cornea gets thinner, weaker, and pushes forward into a cone. This doesn’t happen overnight. It usually starts in the teenage years and progresses slowly, often worsening over 10 to 20 years before stabilizing around age 40. The problem isn’t just that your vision is blurry. It’s that it’s distorted. Straight lines look wavy. Double images appear. Glasses can’t fix this because they sit too far from the eye’s surface. They can’t compensate for the irregular curve of your cornea. That’s where rigid lenses come in.Why Rigid Lenses Work When Glasses Don’t
Soft contact lenses conform to the shape of your cornea. In keratoconus, that means they just mirror the irregularity. Rigid gas permeable (RGP) lenses, on the other hand, are stiff. They don’t bend. They float on a tear film and create a new, perfectly smooth optical surface over your damaged cornea. Think of it like putting a flat glass plate over a bumpy table-the light now travels straight through the glass, not the bumps. Studies show that before fitting, most keratoconus patients have vision around 20/80 or worse. After RGP lenses, many jump to 20/25. That’s not a small improvement. That’s the difference between reading a menu across the room and not being able to see the words at all. There are three main types of rigid lenses used for keratoconus:- RGP lenses: Small (9-10mm), made of oxygen-permeable plastic. Dk values range from 50 to 150, meaning enough oxygen gets through to keep the cornea healthy. They’re the first line of defense for mild to moderate cases.
- Hybrid lenses: A rigid center surrounded by a soft skirt. They offer the clarity of RGP with the comfort of soft lenses.
- Scleral lenses: Larger (15-22mm), they vault over the entire cornea and rest on the white part of the eye (sclera). Between the lens and the cornea is a fluid reservoir that cushions the surface and improves vision dramatically in advanced cases.
How Scleral Lenses Changed the Game
Scleral lenses weren’t always common. Ten years ago, they were expensive and hard to fit. Now, they’re the go-to for stage III and IV keratoconus. Why? Because they don’t touch the damaged cornea at all. The fluid layer underneath acts like a natural bandage, reducing pain and improving stability. Patients who couldn’t tolerate RGP lenses often find relief with sclerals. A 2023 clinical review found that scleral lenses succeed in 85% of advanced keratoconus cases, compared to 65% for traditional RGP lenses. They’re especially helpful if you have corneal scarring, extreme thinning, or dry eyes. The FDA classifies them as Class II medical devices-meaning they require professional fitting and ongoing monitoring. But the results speak for themselves: patients report less glare, sharper focus, and the ability to wear them all day without irritation.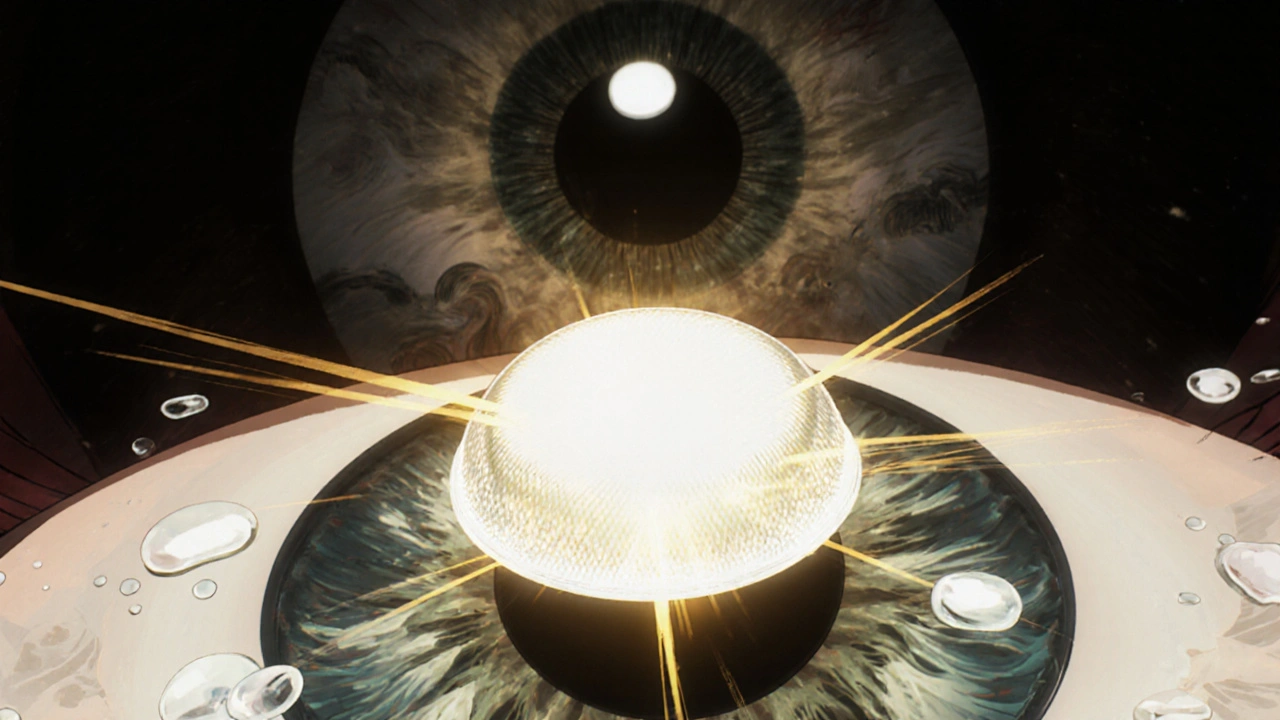
What About Other Treatments?
Rigid lenses don’t stop keratoconus from getting worse. They just help you see better. To actually halt progression, you need corneal cross-linking (CXL). This procedure uses UV light and riboflavin (vitamin B2) to strengthen the collagen bonds in the cornea. It’s the only FDA-approved treatment that stops the cone from getting worse. Studies show it works in 90-95% of cases over five years. But here’s the catch: CXL doesn’t fix your vision. After the procedure, you still need lenses. That’s why most eye doctors now recommend doing both together-CXL to stop the disease, and rigid lenses to restore sight. Other options exist, but they’re less common:- INTACS: Tiny plastic rings inserted into the cornea to flatten the cone. Still, 35-40% of patients need lenses afterward.
- Corneal transplant: Only needed in 10-20% of cases. It’s major surgery. Recovery takes over a year. And even after a transplant, many people still need rigid lenses for the best vision.
What to Expect When You Start Wearing Rigid Lenses
If you’ve never worn contacts before, or especially if you’ve only worn soft ones, rigid lenses feel strange at first. About 30% of patients say they feel like there’s something in their eye during the first week. That’s normal. It’s not pain-it’s awareness. The adaptation process is slow but predictable:- Start with 2-4 hours a day.
- Add 1-2 hours every few days.
- By week 3-4, most people can wear them full-time.
- Foreign body sensation (45% of new wearers)
- Lens awareness (38%)
- Difficulty inserting/removing (32%)
- Lens fogging (25%)
- Decentration (15%)

Who Doesn’t Do Well With Rigid Lenses?
Not everyone is a candidate. About 15-25% of patients with advanced keratoconus can’t get a good fit. Why? Severe scarring, extreme thinning, or a cornea that’s too irregular for the lens to center properly. Chronic dry eye is another dealbreaker-it makes lens wear painful and unstable. In these cases, scleral lenses are the next step. If those don’t work, then it’s time to talk about surgery. But that’s rare. Most people find a solution before it gets that far.The Future of Rigid Lenses for Keratoconus
Technology is moving fast. In 2022, new scleral lens materials hit the market with oxygen permeability ratings over 200-far higher than older versions. That means less risk of corneal swelling, even with long wear. In January 2023, the FDA approved the first digital manufacturing system for custom scleral lenses. Now, your cornea is scanned in 3D, and the lens is built to match your exact shape-down to the micrometer. No more trial-and-error fittings. Fewer visits. Better results. The trend is clear: rigid lenses aren’t going away. With CXL stopping progression and better lenses improving vision, most patients can avoid surgery entirely. The global market for specialty contact lenses is expected to grow from $1.85 billion in 2022 to $2.78 billion by 2027. That’s not just business-it’s proof that these lenses are changing lives.What You Should Do Next
If you’ve been told you have keratoconus:- Get a corneal topography scan. This maps your cornea’s shape and shows how advanced it is.
- Ask about corneal cross-linking. Do it early-it’s most effective before major thinning.
- See a specialist in contact lens fitting. Not all optometrists know how to fit scleral lenses. Look for someone trained in keratoconus care.
- Don’t give up on lenses. The first few weeks are hard. But the clarity you gain is worth it.
Can glasses correct vision in keratoconus?
No, glasses usually can’t fully correct vision in keratoconus. The irregular shape of the cornea causes distorted light bending that glasses, which sit away from the eye, can’t fix. Rigid contact lenses create a smooth new surface over the cornea, which is why they’re the standard for clear vision in moderate to advanced cases.
Are rigid contact lenses uncomfortable?
Initially, yes-about 30% of patients report discomfort during the first week. But this usually fades within 2-4 weeks as the eye adapts. Scleral lenses, which rest on the white of the eye and hold a fluid reservoir, are often more comfortable than traditional RGP lenses, especially for advanced cases.
Do rigid lenses stop keratoconus from getting worse?
No. Rigid lenses only improve vision-they don’t treat the underlying disease. To stop progression, you need corneal cross-linking (CXL), a procedure that strengthens the cornea’s collagen fibers. Most eye doctors now recommend combining CXL with rigid lenses for the best long-term outcome.
How long does it take to adapt to rigid lenses?
Most people adapt within 2 to 4 weeks. Start with 2-4 hours of wear per day and increase by 1-2 hours every few days. By the end of the fourth week, 85% of patients can wear them full-time without discomfort.
What’s the success rate of scleral lenses for keratoconus?
Scleral lenses succeed in about 85% of advanced keratoconus cases (Stage III-IV), compared to 65% for traditional RGP lenses. Their larger size and fluid reservoir make them ideal for irregular, scarred, or thin corneas that other lenses can’t fit properly.
Is corneal transplant the only option if lenses don’t work?
No. Only 10-20% of keratoconus patients eventually need a transplant. Before that point, options like customized scleral lenses, hybrid lenses, or INTACS rings can help. Transplants are reserved for cases with severe scarring, extreme thinning, or lens intolerance that can’t be resolved any other way.
Can keratoconus be cured?
There’s no cure for keratoconus, but it can be effectively managed. Corneal cross-linking stops progression in 90-95% of cases, and rigid contact lenses restore clear vision in the vast majority. With proper care, most people live normal lives without needing surgery.

kora ortiz
November 17, 2025 AT 17:10Just got my first pair of sclerals last month and I can actually see my dog’s face again 😭 No more squinting at the TV or avoiding bright lights. These things are magic. Stop doubting and just go see a specialist.
Jeremy Hernandez
November 18, 2025 AT 02:21Yeah right. Rigid lenses? More like corporate eye care scam. Big Pharma doesn’t want you to know you can fix this with eye yoga and apple cider vinegar. I’ve been doing it for 3 years and my corneas are ‘healing’… or so I’m told by the guy on YouTube who lost his license.
Kathryn Ware
November 19, 2025 AT 17:22Okay I need to say this because I’ve been where you are: it’s HARD at first. I cried the first week. I dropped my lenses in the sink 7 times. I thought I’d never get used to them. But then one morning I woke up and realized I’d looked at my coffee cup without squinting and I didn’t even think about it. That’s when it clicked. Scleral lenses didn’t just give me vision-they gave me back my life. I can drive at night now. I can read my kid’s school emails without zooming in. I can look people in the eye without feeling like I’m hiding. Don’t give up. The first month is brutal. The next 20 years? Worth it. 💪👁️✨
Kiran Mandavkar
November 20, 2025 AT 01:11How convenient that the entire medical-industrial complex has aligned to sell you $800 lenses while ignoring the root cause: your phone addiction. Corneal deformation isn’t genetic-it’s digital. You’re not ‘keratoconus,’ you’re a victim of screen culture. Try looking at the horizon for 20 minutes a day. No lens will fix that.
saurabh lamba
November 20, 2025 AT 02:01My cousin had this. He got transplant. Now he sees better than me. But he’s also a doctor. So maybe it’s not the lens. Maybe it’s just… privilege.
Deb McLachlin
November 21, 2025 AT 23:03Thank you for the comprehensive overview. The distinction between vision correction and disease modification is critical and often misunderstood. I would be interested in seeing longitudinal data on lens durability and patient compliance rates over five-year intervals, particularly regarding scleral lens maintenance protocols.
Kyle Swatt
November 23, 2025 AT 00:28Man… I used to think vision was just about seeing. Turns out it’s about dignity. When you can’t read your own kid’s handwriting, you start feeling like a ghost in your own life. These lenses? They’re not plastic and oxygen-permeable. They’re a bridge back to being human. I didn’t know I was grieving my sight until I got it back. And now I cry every time I put them in. Not from pain. From gratitude.
Shannon Hale
November 24, 2025 AT 00:47Oh my GOD I’m so sick of people acting like this is some miracle cure. You’re just trading one nightmare for another. These lenses cost a fortune, they’re a pain to clean, they pop out if you sneeze, and your eyes feel like sandpaper for months. And don’t even get me started on the ‘specialist’ who charges $600 just to tell you ‘we’ll try this curve.’ I’ve spent $12K and I still can’t watch Netflix without my head tilted. This isn’t medicine. It’s extortion with a side of hope.
Holli Yancey
November 24, 2025 AT 10:48I relate so much to the part about adaptation. I was terrified to even try lenses after my diagnosis. But I’m glad I did. It’s not perfect. Some days are rough. But I don’t feel broken anymore. Just… adjusted.
Jessica Healey
November 25, 2025 AT 10:01So I got my first RGP lenses and my eye doctor said ‘you’ll feel it for a week’ and I was like ‘I got this’ and then I spent 3 days crying in the shower because it felt like a rock in my eye and I wanted to throw them in the trash but my mom was like ‘just wear them 10 minutes a day’ and now I’m like… these are my best friends?? I’m obsessed. I clean them like they’re my baby. I love them. I’m weird.
Levi Hobbs
November 25, 2025 AT 17:10Wait-so if you do CXL, do you still need lenses? Or does it ‘fix’ the shape? I thought it was a cure, not a stopgap. My sister got it done and now she’s saying she doesn’t need contacts anymore…?
Eric Healy
November 26, 2025 AT 16:39My optometrist told me I needed sclerals but I went to another one and he said ‘nah bro you just need better glasses’ and I believed him for 2 years. I’m blind now. Don’t listen to the cheap ones. Find a specialist. Or go blind. Your call.
Tarryne Rolle
November 28, 2025 AT 12:55It’s interesting how we’ve reduced a deeply biological, possibly spiritual disruption of the ocular form to a consumerist problem solvable by silicone and oxygen permeability. We’ve forgotten that the eye is not a camera, and that healing is not merely mechanical. Perhaps the real issue is our refusal to accept impermanence. The cone is not a defect-it’s a revelation. But we’d rather buy a lens than sit with the discomfort.
Gordon Mcdonough
November 28, 2025 AT 22:08Y’all are so naive. The FDA approved this stuff because they’re in bed with lens companies. They don’t want you to know that the real cause is fluoride in the water. I’ve been taking iodine supplements and my corneas are shrinking back. Just sayin’. Also, why do you think they call it ‘keratoconus’? KERA-to-conus. KERA = Kerosene. They’re poisoning us. Wake up.