When you take carbamazepine for epilepsy or nerve pain, you’re not just taking a pill-you’re managing a complex chemical dance inside your body. This drug, whether brand-name Tegretol or a generic version, doesn’t just sit there. It actively changes how your liver processes other medications, and even itself. And when you switch between generic versions, the stakes get higher. For many patients, a simple pharmacy substitution can trigger seizures, dizziness, or worse.
Why Carbamazepine Is More Than Just Another Antiseizure Drug
Carbamazepine works by calming overactive nerve cells, mainly by blocking sodium channels. But its real challenge lies in what it does to your liver enzymes. It’s one of the strongest inducers of CYP3A4, the enzyme responsible for breaking down about half of all prescription drugs. This means carbamazepine doesn’t just affect itself-it can make other medications stop working.
Think about this: if you’re on warfarin for blood thinning, carbamazepine can drop your INR levels so fast that your risk of stroke goes up. Same with birth control pills, cyclosporine after a transplant, or even some HIV drugs. The FDA lists over 20 medications that lose effectiveness when taken with carbamazepine. And here’s the kicker: this effect doesn’t happen right away. It builds over 2-3 weeks, which is why many patients don’t connect their new symptoms to the drug they’ve been taking for months.
Carbamazepine also induces UGT enzymes and P-glycoprotein, which means it affects how drugs are absorbed and cleared through your gut and kidneys. This isn’t just theoretical. In real-world clinics, neurologists see patients with unexplained breakthrough seizures, kidney rejection, or unexpected bleeding-all because carbamazepine was quietly speeding up the metabolism of another drug.
The Narrow Therapeutic Window That Makes Generics Risky
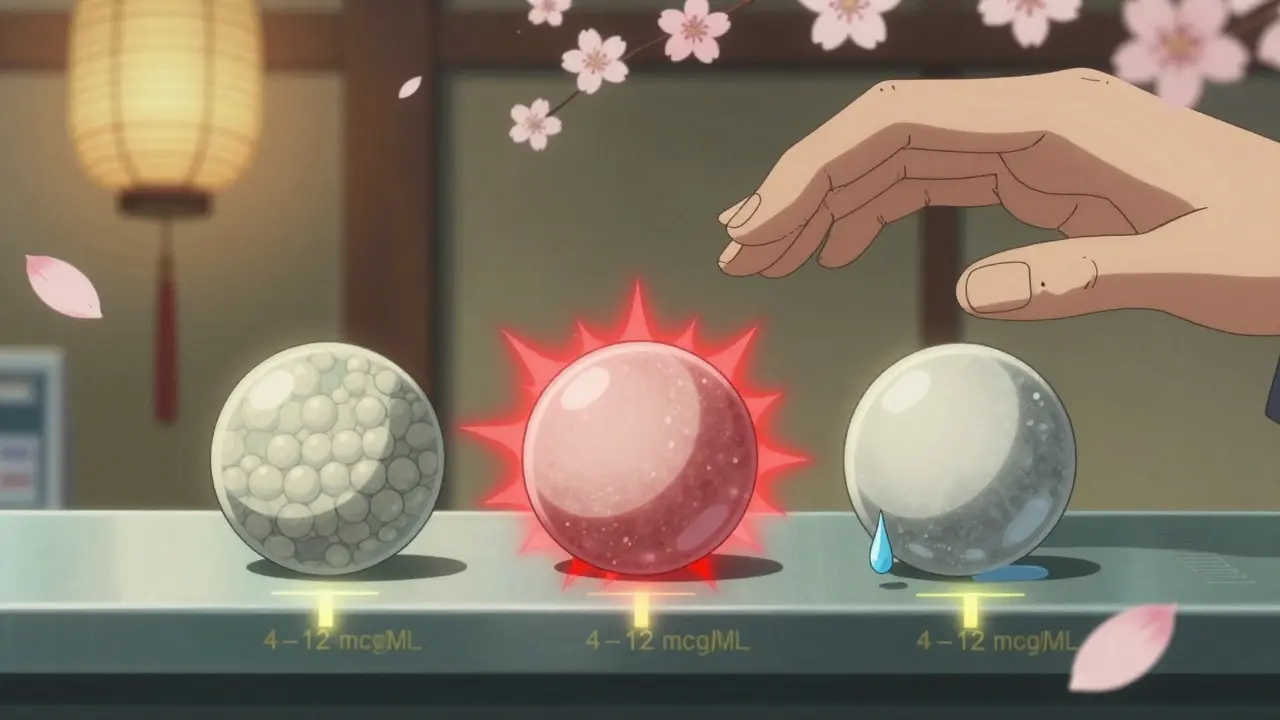
Carbamazepine’s therapeutic range is 4-12 mcg/mL. That’s a tight band. Go below 4, and seizures return. Go above 12, and you risk dizziness, nausea, or even toxic confusion. But here’s the problem: between patients, the same dose can produce levels that vary by 30-40%. That’s huge. And it gets worse with generics.
Generic manufacturers must prove their version is bioequivalent to the brand-meaning it delivers similar peak levels and total exposure in healthy volunteers. But healthy volunteers don’t have epilepsy. They don’t take 5 other drugs. They don’t have liver disease or hormonal fluctuations. A 2018 study of 327 epilepsy patients found that 12.4% had seizures or side effects after switching between generic versions-even though both met FDA standards. Seven percent ended up in the ER.
One patient in a 2023 forum described it plainly: “I stayed on the same dose. My blood test showed my level dropped from 7.2 to 4.8 mcg/mL. Two weeks later, I had five seizures in a week.” That’s not a fluke. It’s a pattern. The European Medicines Agency classifies carbamazepine as a narrow therapeutic index (NTI) drug, meaning tiny differences in absorption can mean big clinical consequences.
Why Not All Generics Are Created Equal
There are 32 approved generic versions of immediate-release carbamazepine tablets and 18 of extended-release forms. Each has different inactive ingredients, coating, bead sizes, and release profiles. For most drugs, this doesn’t matter. For carbamazepine, it does.
Extended-release capsules like Carbatrol or Tegretol XR are designed to release the drug slowly over 12 hours. But some generic versions use different bead sizes or polymer coatings. In patients with gastroparesis (delayed stomach emptying), a slightly faster-releasing capsule can spike levels. A slower one can cause levels to dip below therapeutic range. One nurse on Reddit noted that a specific generic (Nostrum Pharmaceuticals, approved in 2011) had beads that didn’t dissolve well in patients with slow digestion-leading to inconsistent absorption.
Even more concerning: bioequivalence studies are done in 24-36 healthy people over a single dose. But carbamazepine induces its own metabolism. The first dose is different from the 14th. The FDA admits this gap. In 2023, they called carbamazepine extended-release products a “high-priority” for better testing methods because current standards simply don’t capture how the drug behaves in real patients over weeks.
Gender, Genetics, and Hidden Triggers
Men and women metabolize carbamazepine differently. Women have 20-25% higher CYP3A4 activity, meaning they clear the drug faster. This is why women of childbearing age are more likely to have breakthrough seizures when switched between generics. Hormonal changes during the menstrual cycle, pregnancy, or while on birth control can further shift levels unpredictably.
Genetics matter too. About 15% of people of Asian descent carry the HLA-B*1502 gene variant. For them, carbamazepine carries a 10-fold higher risk of Stevens-Johnson Syndrome-a life-threatening skin reaction. The FDA recommends genetic screening before starting, especially for patients of Chinese, Thai, Malaysian, or Filipino descent. Yet many primary care providers still prescribe carbamazepine without checking.
Even within Caucasians, variations in CYP3A4*22 and CYP2C19 genes can mean someone needs 25% less or 30% more of the same dose. Without testing, you’re guessing. And in epilepsy, guessing can be dangerous.

What You Should Do If You Take Carbamazepine
Here’s the practical advice-no fluff, just what works:
- Don’t switch generics unless absolutely necessary. If your current generic works, stay on it. Your neurologist should write “dispense as written” (DAW 1) on the prescription to block automatic substitution.
- Always check the manufacturer. The FDA’s Orange Book lists 12 different companies making 200 mg carbamazepine tablets. If your pharmacy switches brands, ask why. Keep the pill bottle as a reference.
- Get a blood test after any switch. Test your carbamazepine level before switching, then again at 7-10 days and again at 4 weeks. If your level changes by more than 15%, your dose needs adjusting.
- Tell every doctor you see. If you’re on carbamazepine, every provider-even your dentist or primary care doctor-needs to know. Many common drugs (like antibiotics, antifungals, or even some heart meds) interact with it.
- Consider alternatives if you’re Asian or have a history of skin reactions. Levetiracetam or lacosamide are safer first choices for those with HLA-B*1502.
What’s Coming Next
The FDA and EMA are working on better ways to test carbamazepine generics. They’re moving toward steady-state studies-not single-dose-and using real patient data to model how different formulations behave under real conditions. The American Epilepsy Society is developing a free Therapeutic Drug Monitoring Toolkit for clinicians, launching in late 2024. It will include dosing algorithms based on age, sex, weight, and other medications.
Researchers in Glasgow have identified 17 genetic markers that affect how people process carbamazepine. In the next five years, precision dosing using genetic testing will likely become standard. Until then, the safest approach is simple: stick with the same version, monitor your levels, and never assume generics are interchangeable.
Carbamazepine isn’t a drug you can treat like a statin or a blood pressure pill. It’s a high-risk, high-reward tool. And in the world of generics, that means vigilance isn’t optional-it’s essential.