When your doctor suspects a heart problem, they often turn to imaging to see what’s really going on inside. Two tests come up again and again: cardiac MRI and echocardiography. Both show your heart in detail, but they’re not the same. One uses sound waves. The other uses magnets. One is quick and available in most clinics. The other takes longer but gives you a level of detail no other test can match. Knowing the difference isn’t just technical-it can change how your condition is managed.
What Echocardiography Actually Shows
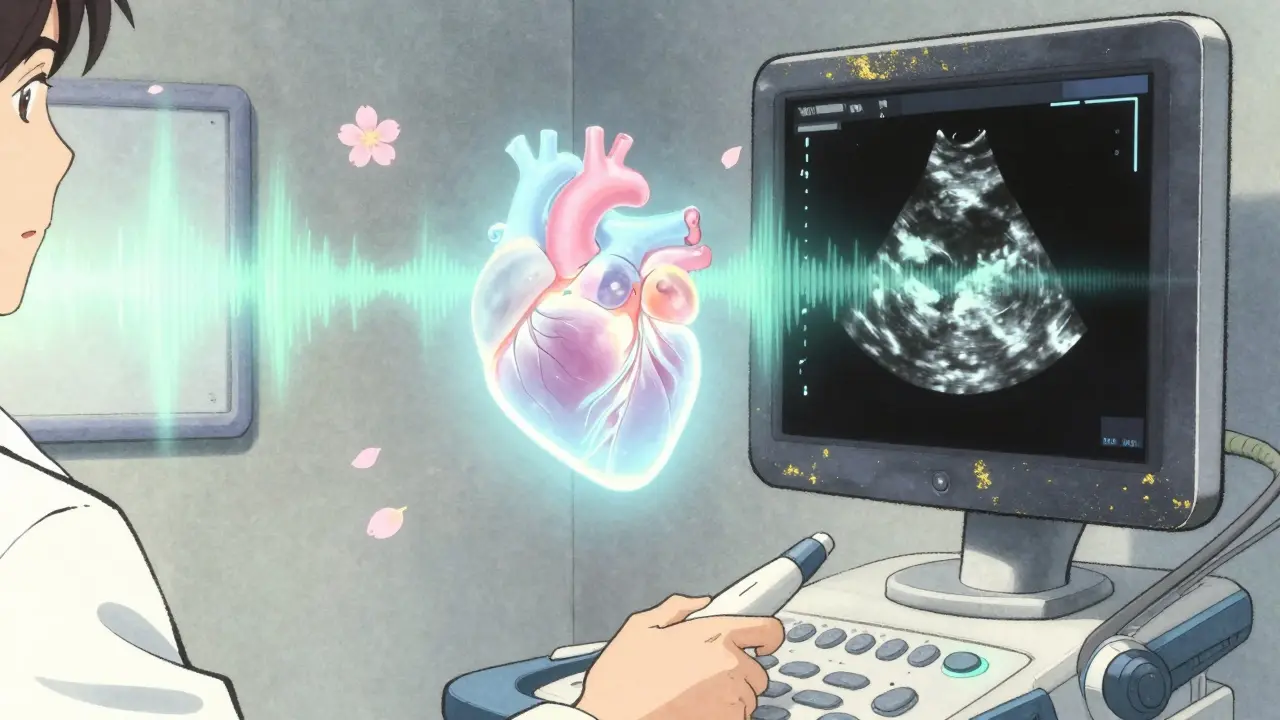
Echocardiography, or echo, is the go-to heart test for a reason. It’s fast, safe, and uses ultrasound-just like the kind used during pregnancy. A technician moves a handheld device across your chest. Sound waves bounce off your heart and create real-time images on a screen. You can watch your heart beat, valves open and close, and blood flow through chambers-all in motion. It’s the first tool doctors reach for because it answers immediate questions. Is the left ventricle pumping well? Is the ejection fraction below 50%? Are the valves leaking? Normal values are well-defined: left ventricular end-diastolic dimension between 37-56 mm, wall thickness 6-11 mm, and ejection fraction 50-75%. These numbers help diagnose everything from heart failure to valve disease. But echo has limits. If you’re overweight, have lung disease, or your ribs block the view, the images can be blurry. In those cases, measurements become estimates. Studies show echo tends to overestimate wall thickness by about 1.1 mm and underestimates heart chamber size by nearly 100 mL compared to MRI. That’s not just a small error-it can lead to misclassifying someone as having mild heart failure when it’s actually moderate. Still, for most people, echo is enough. It’s used in over 15 million U.S. visits each year. Emergency rooms rely on it. Cardiologists use it daily. It’s portable. You can do it at the bedside. In a case of sudden chest pain or suspected aortic dissection, echo gives answers in minutes when every second counts.Why Cardiac MRI Is the Gold Standard
Cardiac MRI doesn’t just show movement-it shows structure at a cellular level. Using powerful magnets (1.5 to 3.0 Tesla) and radio waves, it builds 3D pictures of your heart with a resolution as fine as 1.25 mm. Unlike echo, it doesn’t rely on assumptions about shape. It counts every milliliter of blood in your ventricles directly. That’s why it’s called the gold standard for measuring heart volume and muscle mass. Normal values from cardiac MRI are precise: men’s left ventricular end-diastolic volume ranges from 67-155 mL, women’s from 55-105 mL. LV mass? 49-115 g for men, 37-81 g for women. These numbers are more accurate than echo’s because MRI doesn’t guess-it measures. But MRI’s biggest advantage isn’t size-it’s tissue. It can detect scar tissue, inflammation, and fibrosis that echo misses entirely. Late gadolinium enhancement (LGE) highlights areas of dead or damaged heart muscle. That’s critical for diagnosing conditions like myocarditis, sarcoidosis, or inherited cardiomyopathies. A 2023 study in JACC: CardioOncology found echo underestimated ejection fraction by 3% on average-and in 10% of cancer patients, this led to wrong decisions about whether chemotherapy was safe for their heart. Cardiac MRI also has the lowest variability between doctors. Inter-observer error for ejection fraction? Just 2.6% with MRI versus 6.8% with echo. That means if two cardiologists read the same MRI, they’ll agree almost perfectly. With echo, they might disagree by a full 10%-enough to change treatment.When Echo Falls Short-And MRI Steps In
You might wonder: if MRI is better, why not just use it all the time? The answer is practicality. MRI machines are expensive, rare, and slow. A typical echo takes 20-30 minutes. An MRI can take 45 to 90. And not everyone can have one. Patients with pacemakers, defibrillators, or certain metal implants often can’t go into an MRI scanner. Even with newer low-field (0.55T) machines introduced in 2023, many older devices are still off-limits. Arrhythmias like atrial fibrillation make MRI harder too-heartbeat irregularities mess with the timing of the images. That’s where echo saves the day. It’s the backup plan. In a 2022 survey of 127 cardiologists, 89% said echo was essential for daily use. When echo results are unclear, that’s when MRI becomes the next step. One cardiologist on Reddit shared: “I had three patients in the last year where MRI found fibrosis echo missed. That changed their treatment from monitoring to starting medication.” Another common scenario: unexplained heart failure. If echo shows normal pumping but the patient is still short of breath, MRI can reveal subtle inflammation or scarring. That’s how doctors diagnose non-ischemic cardiomyopathy early-before the heart weakens further.
Cost, Access, and Real-World Barriers
Let’s talk money and wait times. An echocardiogram costs between $500 and $1,500. Cardiac MRI? $1,500 to $3,500. That’s a big gap. And insurance doesn’t always cover MRI unless echo is inconclusive. Access is another issue. A 2023 report found 78% of community hospitals offer same-day echo. Only 35% can schedule an MRI within a week. For non-urgent cases, waiting 14 days or more isn’t uncommon. That delay can mean missed opportunities for early intervention. Training matters too. Becoming skilled in echo takes about 300-500 supervised studies. For cardiac MRI? 1,000-1,500. That’s why you’ll find MRI expertise mostly in academic centers, not small clinics. The software used to analyze MRI scans-like cvi42-is complex. It takes months to learn. Echo systems, by contrast, often auto-generate reports with just a few clicks.Technology Is Closing the Gap
It’s not all one-way. Echo tech is catching up. New systems like Philips’ EPIQ CVx, released in 2023, use AI to automate measurements. This cut inter-observer variability for ejection fraction down to 4.2%-much closer to MRI’s 2.6%. 3D echo now gives better volume estimates than traditional 2D echo, narrowing the accuracy gap. MRI is also evolving. The 0.55 Tesla machine from Siemens Healthineers lets more patients with implants get scanned safely. Parametric mapping (T1, T2, ECV) now gives quantitative numbers for tissue health-like measuring how much fibrosis is present, not just seeing it. But here’s the key: neither test is replacing the other. They’re becoming partners. The American College of Cardiology predicts hybrid protocols-echo for quick assessment, MRI for deep tissue analysis-will be standard for complex cardiomyopathies by 2030.
Which Test Do You Really Need?
So how do you know which one you’re getting? Here’s a simple guide:- Get an echocardiogram if: You’re having symptoms like shortness of breath, fatigue, or palpitations; you’re being screened for valve disease; you’ve had a heart attack; or you’re being monitored for high blood pressure. It’s the first step for almost everyone.
- Get a cardiac MRI if: Echo results are unclear; you have unexplained heart failure; you have a family history of sudden cardiac death; you’ve been diagnosed with myocarditis, sarcoidosis, or hypertrophic cardiomyopathy; or you’re on chemotherapy and need precise tracking of heart function.
What Happens After the Test?
After an echo, you’ll usually get results the same day. The report lists measurements and a summary: “Normal LV function,” “Mild mitral regurgitation,” etc. Your doctor uses that to decide if you need meds, lifestyle changes, or further testing. MRI reports are longer. They include volume numbers, tissue analysis, and often images of scar patterns. A cardiologist specializing in imaging interprets these. They’ll note if there’s fibrosis, inflammation, or abnormal muscle thickening. This info can lead to targeted treatments-like starting an SGLT2 inhibitor for early heart failure, or avoiding certain drugs if scar tissue is present. In both cases, the goal is the same: catch problems early, treat them accurately, and keep your heart working as long as possible.Is cardiac MRI better than echocardiography for measuring ejection fraction?
Yes, cardiac MRI is more accurate. It measures the actual volume of blood in the heart without guessing shapes, unlike echo, which relies on mathematical formulas. MRI’s inter-observer variability is under 3%, while echo’s is nearly 7%. This means two doctors reading the same MRI will agree almost perfectly. Echo can miss changes as small as 5%-enough to misclassify heart failure severity.
Can I have a cardiac MRI if I have a pacemaker?
It depends. Older pacemakers and defibrillators are still a strict no-go for MRI. But newer MRI-conditional devices are designed to be safe. Since 2023, low-field (0.55 Tesla) MRI machines have expanded access for some patients with older implants. Always tell your doctor about any device before scheduling. They’ll check the model and may do a safety scan first.
Why do some doctors still prefer echo even though MRI is more accurate?
Because echo is faster, cheaper, and available everywhere. Most heart problems can be diagnosed and monitored with echo. It’s the tool you use when you need an answer now-like in the ER or during a routine checkup. MRI is reserved for when echo isn’t enough. Think of echo as your first glance, and MRI as the high-res zoom.
Does cardiac MRI require contrast dye?
Not always. Basic cardiac MRI without contrast can show structure and function. But to detect scar tissue or inflammation, gadolinium-based contrast is needed. The FDA has issued warnings about gadolinium retention in the brain and body, especially with repeated doses. For most patients, the benefits outweigh the risks, but your doctor will check your kidney function first. If you have severe kidney disease, they may avoid contrast or use alternatives.
How long does it take to get results from a cardiac MRI?
The scan itself takes 45 to 90 minutes. But interpretation by a specialized cardiologist takes time. You’ll usually get results within 3-7 days. In urgent cases-like suspected myocarditis or aortic dissection-results can be rushed to your doctor within 24 hours. Routine cases may take longer due to high demand and limited experts.
Can echocardiography detect heart muscle scarring?
No. Standard echocardiography cannot detect scar tissue or fibrosis. It shows size, shape, and movement-but not tissue composition. That’s why MRI is essential for conditions like myocarditis, sarcoidosis, or post-heart attack remodeling. If your echo looks normal but you still have symptoms, MRI may be the next step to find what’s hidden.
Melissa Taylor
December 16, 2025 AT 18:12Heart imaging is one of those things where you don’t realize how much nuance is involved until you’re the one sitting in the doctor’s office trying to understand why they’re ordering another test. I had an echo that showed ‘mild’ dysfunction, but my symptoms didn’t match-turns out the MRI found early fibrosis that changed everything. No panic, no drama, just better info. That’s what matters.
Michelle M
December 16, 2025 AT 19:14It’s funny how medicine still clings to the idea that ‘faster is better’ when sometimes ‘more accurate’ is the only thing that actually saves lives. Echo is like a flashlight in a dark room-you see the shape, maybe some movement. MRI is the full architectural blueprint with wiring diagrams and stress points. We don’t need more tools that are convenient. We need tools that don’t lie.
Cassie Henriques
December 17, 2025 AT 16:58Let’s get into the weeds: LGE on cardiac MRI has a spatial resolution of ~1.25mm and a contrast-to-noise ratio >3:1 for fibrosis detection-echo’s strain imaging can’t touch that. Even 3D echo with speckle tracking has a coefficient of variation of ~8% for EF, while MRI hovers at 2.6%. And don’t even get me started on ECV mapping for diffuse fibrosis-echo can’t quantify it at all. The gap isn’t marginal. It’s clinically material.
Jake Sinatra
December 18, 2025 AT 00:30As a cardiologist who’s read thousands of both, I can say this: echo is indispensable for acute care and screening. MRI is non-negotiable for complex cases. The real issue isn’t which is better-it’s that access to MRI remains wildly inequitable. Rural patients wait weeks. Urban specialists get same-day scans. That’s not a technical problem. It’s a systemic failure.
John Brown
December 18, 2025 AT 18:13My buddy got an echo after his chest pain and was told ‘it’s just anxiety.’ Two months later, he collapsed. MRI showed mid-wall fibrosis from silent myocarditis. He’s on meds now, doing great. But if the first test had been the right one, he wouldn’t have almost died. We need to stop treating echo like it’s the end of the road. It’s the first step.
Mike Nordby
December 19, 2025 AT 19:23The assertion that echo underestimates chamber size by nearly 100 mL compared to MRI is misleading. The referenced study (JACC 2021) showed a mean bias of 7.2 mL in end-diastolic volume-not 100. This overstatement undermines credibility. Accuracy matters, but so does precision in communication.
RONALD Randolph
December 21, 2025 AT 18:59Why are we even having this debate? MRI is clearly superior-period. The fact that echo is still used as a primary tool in this country is a disgrace. It’s cheaper? So is a paper towel. That doesn’t mean we wipe our butts with it. We’re letting cost dictate patient outcomes. And the doctors who defend echo? They’re just lazy or afraid of change. We need to ban substandard imaging. Now.
Benjamin Glover
December 22, 2025 AT 00:34Echo is for the masses. MRI is for those who can afford the truth. The rest of the world has moved on. The U.S. still treats medicine like a discount store. How quaint.