Why Medication Safety at Home Matters More Than You Think
Every year, 1.9 million children under six in the U.S. are exposed to medications they weren’t supposed to touch. Most of these incidents happen in the home-when a grandparent leaves a pill bottle on the counter, or a toddler climbs up to reach a purse on a chair. It’s not just kids. Older adults taking five or more pills a day are at high risk for dangerous interactions, missed doses, or accidental overdoses. The truth? Medication errors in the home are one of the most preventable health crises we ignore.
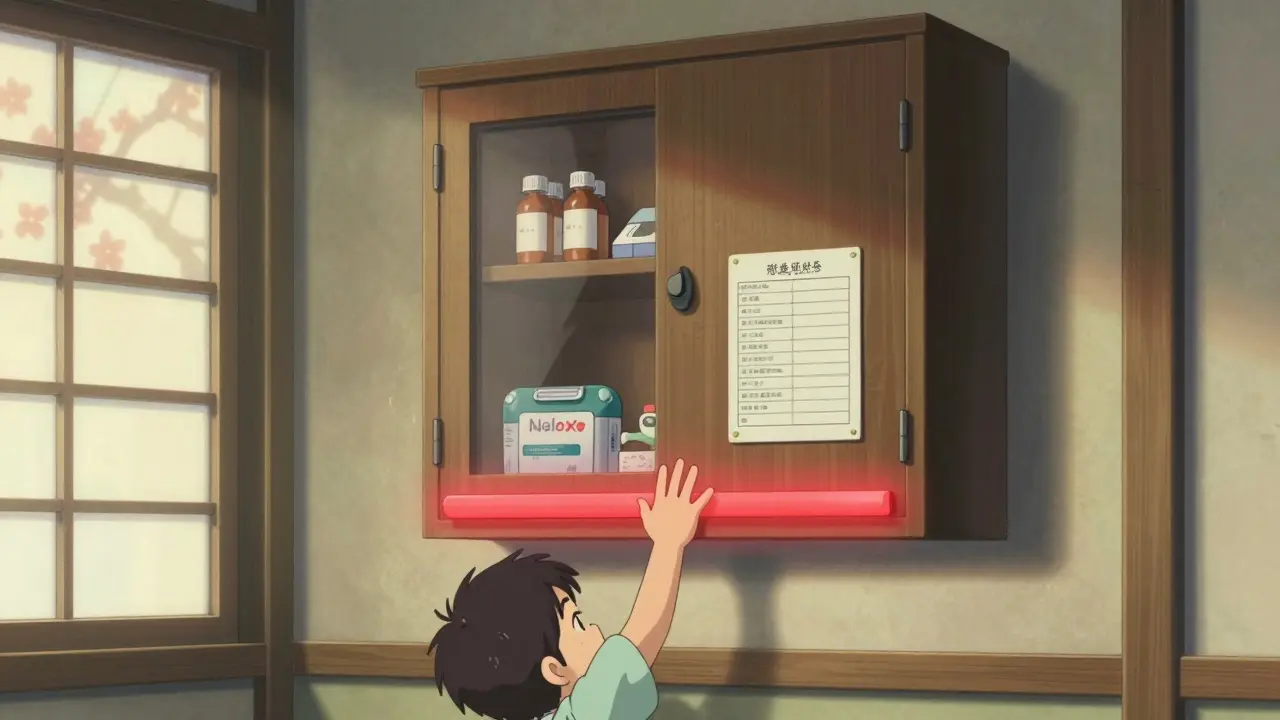
Store Medications Like They’re Valuables-Not Afterthoughts
Keeping medicine in the bathroom is a common mistake. Humidity from showers and sinks can ruin pills and liquids, making them less effective or even unsafe. The CDC says to keep all medications in their original containers with child-resistant caps tightly closed. But that’s not enough.
Store everything up and away-meaning above eye level and out of reach. A locked cabinet in a bedroom or closet is ideal. If you have opioids, painkillers, or sedatives in the house, lock them separately. Dr. Lorraine Kelley-Quon from Children’s Hospital Los Angeles says: “If there are opioids in the house, parents need to be aware of the signs-small pupils, slowed breathing, lethargy.” Keep naloxone (Narcan) on hand if you’re caring for someone on opioids.
And don’t forget purses, bags, or nightstands. A 2023 study found that 25% of kids who got into medicine did so because a caregiver left a bag on the kitchen counter. Treat every pill bottle like a loaded gun-lock it, hide it, and never leave it unattended.
Know the Five Rights of Medication Administration
Before giving any medicine, ask yourself these five questions:
- Right child? Is this medicine meant for the person you’re giving it to?
- Right medication? Does the name on the bottle match what the doctor prescribed?
- Right dose? Are you using the measuring tool that came with it? Never use a kitchen spoon.
- Right route? Is it meant to be swallowed, applied to the skin, or inhaled?
- Right time? Are you giving it at the correct interval-every 8 hours, once daily, after meals?
These aren’t just hospital rules. They’re lifesavers at home. A 2022 study showed that families who used the Five Rights reduced medication errors by over 50%. Even if you’ve given the same medicine for years, double-check every time. Names change. Doses change. People change.
Build a Master Medication List-And Keep It Updated
Write down every single thing your family takes. Not just prescriptions. Include vitamins, herbal supplements, over-the-counter painkillers, cough syrups, and even topical creams. A 2023 AARP survey found that 73% of caregivers say managing medications is their biggest stressor-and 42% admit they’ve made at least one mistake in the past year. Most of those mistakes happened because they forgot what someone was taking.
Use a simple spreadsheet or notebook. Include:
- Medication name (brand and generic)
- Dosage and frequency
- Reason for taking it
- Start date
- Side effects to watch for
- Prescribing doctor’s name
Keep a printed copy on the fridge. Share it with every caregiver-babysitters, grandparents, nurses. Bring it to every doctor’s appointment. The American Pharmacists Association recommends a “brown bag” review every six months: dump all your meds into a bag and take them to your pharmacist. They’ll spot duplicates, interactions, or drugs you no longer need.

Use Tools That Actually Work
Not all pill organizers are created equal. A 7-day compartment organizer with morning/afternoon/evening slots works well for most families. But if someone’s taking 10 pills a day, a simple box won’t cut it.
Try these proven tools:
- Color-coded tape: Use painter’s tape to mark pill bottles by color-red for blood pressure, blue for cholesterol. One Reddit caregiver reported a 60% drop in errors after doing this.
- Digital reminders: Apps like Medisafe or MyTherapy send alerts and track doses. But if your parent or grandparent isn’t tech-savvy, don’t force it. 27% of older adults abandon apps within three months.
- Oral syringes: For liquids, never use a measuring cup. Use the syringe that came with the medicine. A 2022 study found syringes cut dosing errors by 47%.
- Smart dispensers: Devices like Hero or MedMinder automatically dispense pills and notify caregivers if a dose is missed. They’re expensive, but worth it if someone’s on complex meds.
For kids, use a dosing syringe even if the bottle says “use the cup.” Kids spit out liquid. They don’t swallow it evenly. A syringe lets you control exactly how much goes in.
What to Do When a Dose Is Missed
It happens. You’re rushing, you’re tired, you forget. The rule isn’t “double up.” It’s this:
If you miss a dose, give it as soon as you remember. Then, give the next dose at the normal time-even if it’s sooner than usual. Never give two doses at once unless a doctor tells you to. Overdosing on common meds like acetaminophen (Tylenol) can cause liver failure. One extra pill can be deadly.
Keep a note in your medication list: “If I miss a dose, I’ll give it within 2 hours. After that, skip it.” Write it down. Stick it on the fridge. That’s your backup plan.
Dispose of Old or Unused Meds the Right Way
Don’t flush pills down the toilet. Don’t throw them in the trash where a kid or pet might dig them out. The FDA recommends two safe options:
- Use a drug take-back program. Many pharmacies and police stations have drop boxes.
- If no take-back is nearby, mix pills with coffee grounds or cat litter in a sealed bag, then throw it in the trash.
Get rid of expired, unused, or discontinued meds every 3-6 months. A cluttered medicine cabinet isn’t just messy-it’s dangerous.

Review Medications with a Pharmacist Every 6 Months
Doctors don’t always know what’s in your medicine cabinet. Pharmacists do. They’re trained to spot interactions, duplicate prescriptions, and unnecessary drugs.
The American Society of Health-System Pharmacists says regular pharmacist reviews reduce adverse drug events by 27%. That’s huge. For seniors, the American Geriatrics Society warns that anticholinergic drugs-often found in sleep aids, allergy meds, and bladder pills-can increase fall risk by 50%. Many of these can be safely stopped.
Ask your pharmacist: “Is every medicine still needed?” “Is there a safer alternative?” “Could any of these be causing dizziness or confusion?”
Teach Your Family-Even the Kids
Children don’t understand what medicine is. But they can learn: “This is not candy.” “Only Mommy or Daddy gives these.” “Never touch the bottle.”
Make it part of your routine. Show your child how you take your pill. Say it out loud: “This is my blood pressure medicine. I take it at breakfast.” Make it normal. Make it clear.
And teach older kids to be helpers-not risk-takers. If they’re old enough to read, show them the label. Let them hand you the pill bottle. It builds responsibility and awareness.
Know the Poison Control Number-And Save It Everywhere
One of the biggest gaps in home medication safety? People don’t know the Poison Control number: 1-800-222-1222.
The CDC says 60% of households don’t know it. That’s unacceptable. Save it in your phone. Write it on the fridge. Put it on the back of your medication list. If you ever suspect someone has taken too much medicine-don’t wait. Call immediately. Even if you’re not sure. It’s free. It’s confidential. And it saves lives.
Final Thought: It’s Not Perfect-But It’s Possible
You don’t need to be a nurse to keep your family safe. You just need to be consistent. Lock the meds. Write the list. Use the syringe. Call the pharmacist. Teach your kids. Know the number.
It takes 45 to 90 minutes to set up a full system. Then, it’s 5 minutes a day to stay on track. The payoff? No more panic calls at 2 a.m. No more ER visits for accidental overdoses. No more guilt over a missed pill.
Your family’s safety isn’t about perfection. It’s about building habits that stick. Start today. One step at a time.
What should I do if my child swallows medicine they weren’t supposed to?
Call Poison Control immediately at 1-800-222-1222. Don’t wait for symptoms. Don’t try to make them vomit. Have the medicine bottle ready when you call-so you can tell them the name, dose, and how much was taken. Keep the number saved in your phone and posted on the fridge.
Can I store all my medications in one place?
Yes-but only if it’s locked and out of reach. Never store medications in the bathroom or near food. Use a locked cabinet in a bedroom or hallway. Keep opioids and controlled substances in a separate, locked container. Always keep medicines in their original bottles with child-resistant caps.
Is it safe to use a pill organizer for every medication?
Most medications are fine in a pill organizer, but some shouldn’t be removed from their original packaging. Liquid antibiotics, pills that break down in air (like nitroglycerin), and medications that need refrigeration should stay in their original containers. Always check with your pharmacist before transferring any drug.
How often should I review my family’s medications?
Every six months. Bring all medications-including vitamins and supplements-to your pharmacist for a “brown bag” review. Also, schedule a medication check-up with your doctor at least once a year. This helps catch duplicates, unnecessary drugs, and dangerous interactions, especially for older adults.
Are smart medication dispensers worth the cost?
If someone in your family takes five or more medications daily, has memory issues, or has had a near-miss with a missed or double dose, then yes. Smart dispensers like Hero or MedMinder automatically release pills, send alerts, and notify caregivers if a dose is skipped. They cost $200-$500 upfront, but can prevent costly ER visits and hospitalizations.
What’s the biggest mistake families make with medications?
Leaving pills unsecured. Whether it’s on the counter, in a purse, or in a drawer without a lock-unsecured meds are the #1 cause of accidental poisonings in kids and the #2 cause of errors in seniors. Locking them away-even if it’s inconvenient-is the single most effective thing you can do.
Henriette Barrows
December 30, 2025 AT 10:56This is actually the most practical guide I've seen on this topic. I used to keep all my mom's meds in the bathroom drawer until her blood pressure pills got moldy. Now everything's locked in her bedroom cabinet with a color-coded tape system. Game changer.
Alex Ronald
January 1, 2026 AT 09:51For anyone using pill organizers, remember: some meds degrade fast when removed from original packaging. Nitroglycerin, antibiotics, and refrigerated meds should stay put. Always check with your pharmacist before transferring anything.
Jim Rice
January 2, 2026 AT 16:10Locking meds? That's so extra. My kid's never touched anything. You people act like every household is a drug den. I just keep things on the counter. It's fine.
Fabian Riewe
January 2, 2026 AT 16:28Jim, I get where you're coming from, but statistically, 1.9 million kids get into meds every year. That's not paranoia, that's probability. I used to think the same way until my niece swallowed half a bottle of Benadryl from my nightstand. Took 45 minutes to get to the ER. Don't wait for the worst-case scenario.
Nicole K.
January 3, 2026 AT 11:08If you can't even lock up your medicine you don't deserve to be a parent. My 3-year-old knows not to touch the blue bottle because I told him it's not candy. It's called parenting. Not rocket science.
Sharleen Luciano
January 3, 2026 AT 23:05Color-coded tape? Really? That's your solution? You're treating medication like a kindergarten art project. A proper medication management system requires professional-grade labeling, digital integration, and compliance tracking-not sticky notes from Home Depot.
Jasmine Yule
January 4, 2026 AT 11:14Smart dispensers are worth it if you're juggling 5+ meds. My grandma had a Hero device. It called me when she missed a dose. Saved her from a hospital trip last winter. $300 is nothing compared to a 3-day ER stay.
Amy Cannon
January 6, 2026 AT 07:13It's fascinating how Western societies have turned medication into this high-stakes ritual. In my family in Kerala, we'd just take what the doctor said without lists or alarms. Maybe we're missing something... or maybe we're just less anxious.
Samar Khan
January 6, 2026 AT 20:54Ugh I hate when people act like they're saving lives by putting pills in a drawer. My aunt died from an overdose because she took two pills because she forgot. But guess what? She was also on 12 different meds and her doctor never reviewed them. So yeah, lock your stuff... but also, maybe your doctor is the real problem? 🤷♀️
Himanshu Singh
January 7, 2026 AT 10:56Great tips! I use Medisafe app for my dad’s meds. But he keeps forgetting phone password. So I print out the schedule and put it on fridge with big letters. Works better than app for him. Also, always use syringe for liquid meds. Spoon is a myth.
Greg Quinn
January 9, 2026 AT 01:35Medication safety isn't about control. It's about respect. Respect for the power of chemicals, respect for the vulnerability of the body, respect for the fact that we're all just one distracted moment away from disaster. The system isn't perfect, but the intention is what matters.
Joe Kwon
January 10, 2026 AT 23:46Agree with the pharmacist review point. My dad had three duplicate prescriptions and two anticholinergics he didn't need. Pharmacist caught it during a brown bag review. He stopped one pill and his balance improved instantly. These folks are unsung heroes.
Russell Thomas
January 12, 2026 AT 19:15So let me get this straight... we need a spreadsheet, a locked cabinet, a smart dispenser, color-coded tape, a syringe, a poison control bookmark, AND a 6-month review... just to not die from Tylenol? I'm starting to think the pharmaceutical industry designed this whole system to keep us terrified and buying more stuff.
Teresa Rodriguez leon
January 13, 2026 AT 23:10My husband forgot to lock the meds after his surgery. Our 2-year-old got into the opioids. We called Poison Control. They told us to watch for slow breathing. We spent 3 hours in the ER. I haven't slept since. Don't be that person. Lock it. Now.