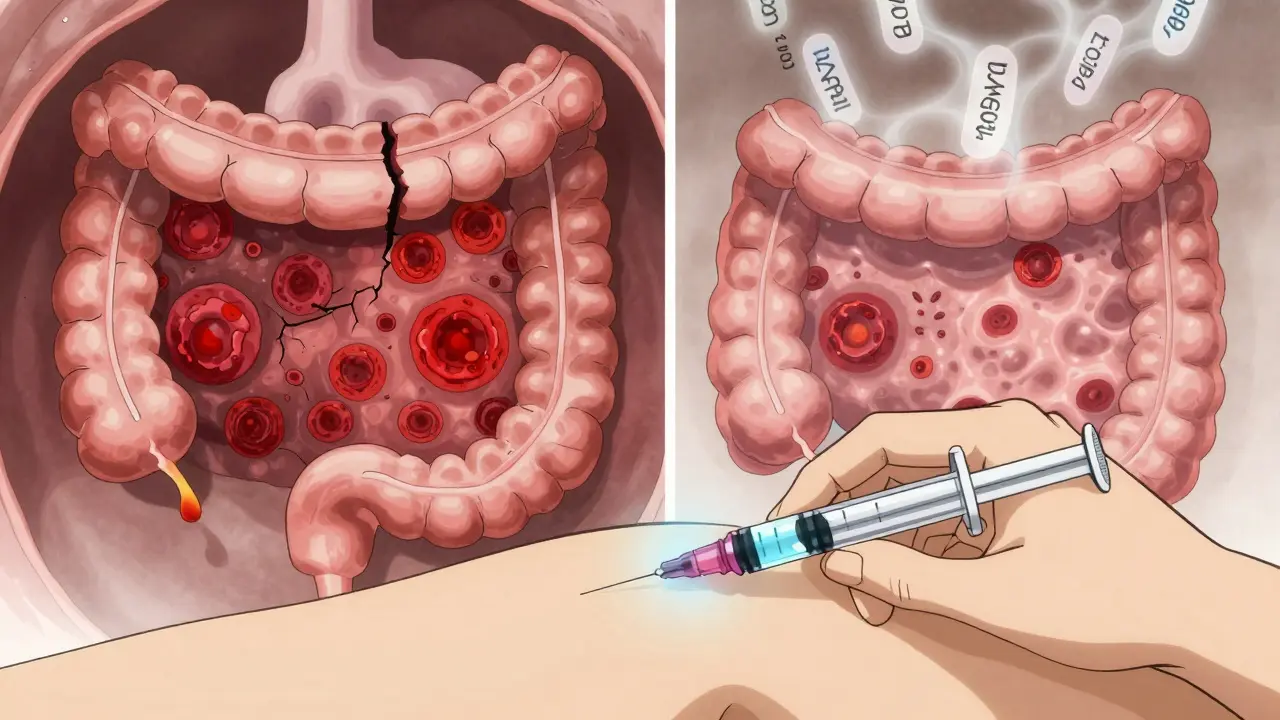
When your body turns against itself, eating a meal can feel like a battle. For people with Crohn’s disease, the digestive tract becomes a war zone - not from infection, but from the immune system attacking its own tissue. This isn’t just occasional stomach upset. It’s chronic, unpredictable inflammation that can strike anywhere from the mouth to the anus, most often in the lower part of the small intestine and the beginning of the colon. About 780,000 people in the U.S. live with this condition, and while there’s no cure, the way we treat it has changed dramatically in the last 25 years.
What Makes Crohn’s Disease Different?
Crohn’s isn’t like a stomach bug that clears up in a few days. It’s a lifelong condition that flares up and then goes quiet, sometimes for months or even years. The inflammation doesn’t just sit on the surface - it digs deep into the walls of the gut, causing cracks, tunnels (called fistulas), and scar tissue that narrows the intestine (strictures). Up to half of people with Crohn’s develop strictures within 10 years. About a third develop fistulas, which can lead to painful abscesses or infections that need surgery. What triggers this? It’s a mix of genes, immune misfires, and environment. Over 200 genes have been linked to Crohn’s, with the NOD2 gene mutation found in 30-40% of people with a family history. But having the gene doesn’t mean you’ll get the disease. Smoking, diet, antibiotics in childhood, and even where you live (higher rates in cities and northern climates) all play a role. The immune system starts seeing harmless gut bacteria as enemies, sending T-cells and other immune fighters into the intestinal wall. They release chemicals like TNF-alpha, IL-12, and IL-23 - inflammatory signals that keep the fire burning even when there’s no real threat.How Biologics Stopped the War
Before biologics, treatment was a game of damage control. Steroids gave quick relief but couldn’t be used long-term - they cause bone loss, diabetes, and mood swings. Immunosuppressants like azathioprine worked slowly and carried risks of liver damage and cancer. The real shift came in 1998 with the approval of infliximab (Remicade), the first biologic drug for Crohn’s. Biologics are made from living cells, not chemicals. They’re designed to block specific parts of the immune response. Anti-TNF drugs like infliximab, adalimumab (Humira), and certolizumab pegol (Cimzia) latch onto TNF-alpha and neutralize it. That cuts inflammation fast. Studies show 30-40% of patients go into remission on anti-TNFs, compared to just 15-20% on placebo. That’s not just feeling better - it’s healing the gut lining. Mucosal healing, where the intestinal wall actually repairs itself, happens in 40-60% of patients on biologics, versus 20-30% on older drugs. But not everyone responds to anti-TNFs. That’s where newer biologics come in. Vedolizumab (Entyvio) works differently. Instead of blocking a chemical signal, it stops immune cells from even reaching the gut. It targets a molecule called α4β7 integrin - the “address label” that tells white blood cells to head to the intestines. Because it only blocks gut traffic, it’s less likely to cause infections elsewhere in the body. In trials, 75% of its effect is focused on the bowel, making it a top choice for people with other autoimmune conditions like multiple sclerosis. Then there’s ustekinumab (Stelara), which blocks IL-12 and IL-23 - two key cytokines driving the inflammation. In the UNITI trials, about 40% of patients achieved remission in just 8 weeks. And it lasts. Half of those patients stayed in remission after a year.Choosing the Right Biologic
There’s no one-size-fits-all. The choice depends on your disease pattern, other health issues, and even your lifestyle.- Anti-TNFs (infliximab, adalimumab): Fast-acting. Good for severe flares, fistulas, or deep ulcers. Infliximab is given as an infusion every 8 weeks. Adalimumab is a self-injection every 2 weeks. Both can lose effectiveness over time as the body builds antibodies against them - about 30-46% of patients do.
- Vedolizumab: Slower to work - takes 10 to 14 weeks to show results - but much lower risk of antibodies. Ideal if you’ve had a bad reaction to anti-TNFs or want to avoid systemic immune suppression.
- Ustekinumab: Works well for people who didn’t respond to anti-TNFs. Given as an injection every 8 or 12 weeks after an initial dose. Good long-term results with fewer infections than anti-TNFs.
Monitoring and Managing Side Effects
Biologics aren’t risk-free. They suppress parts of your immune system, so you’re more vulnerable to infections like tuberculosis, hepatitis B, and even rare fungal infections. That’s why everyone gets tested before starting: a TB skin test, hepatitis panel, and sometimes a heart check. If you’ve had cancer or heart failure, some biologics aren’t safe. The most common side effect? Injection site reactions - redness, itching, or swelling where you give yourself the shot. About 20-30% of adalimumab users deal with this. It usually fades over time. Infusion reactions during infliximab treatments - like fever, chills, or rash - happen in about 10% of cases. Most are mild and managed with pre-meds like antihistamines. Serious infections occur in 12-15 out of every 100 patients per year, compared to 8-10 on older drugs. That’s why doctors monitor you closely. Blood tests every few months check for signs of infection or liver trouble. Another hidden issue: infusion anxiety. About 1 in 4 patients feel panic or dread before an infusion. It’s not just fear of needles - it’s the weight of knowing this treatment is life-changing but also invasive. Some clinics now offer cognitive behavioral therapy sessions to help patients cope.Therapeutic Drug Monitoring: The Secret Weapon
One of the biggest advances in Crohn’s care isn’t a new drug - it’s how we use the ones we have. Therapeutic drug monitoring means checking the level of the biologic in your blood and measuring whether your body is making antibodies against it. For infliximab, the sweet spot is 3-7 μg/mL. Below 3, you’re likely to relapse. Above 7, you risk side effects without extra benefit. For adalimumab, 5-12 μg/mL is ideal. If levels are low and you’re still having symptoms, your doctor can increase the dose or shorten the interval. If antibodies are high, switching to a different biologic may be better than trying to boost the dose. Data from the American Gastroenterological Association shows patients who get their levels checked have 3.5 times higher remission rates than those who don’t. It’s not guesswork - it’s precision medicine.
Real Lives, Real Outcomes
People on biologics aren’t just statistics. On Reddit’s Crohn’s community, one user wrote: “After 15 bowel movements a day, infliximab brought me down to 2 in three infusions. I went back to work. I slept through the night.” But it’s not perfect. Another user developed a lupus-like reaction on Humira and needed six months of steroids to recover. That’s rare - but it happens. A 2023 survey of over 1,200 patients found:- 78% felt their quality of life improved
- 85% stopped or cut back on steroids
- 72% had fewer hospital visits
- 68% were able to keep their jobs
- But 65% struggled with cost - 40% skipped doses because of price
What’s Next?
The future is promising. New drugs like mirikizumab (an IL-23 blocker) and ozanimod (a pill that traps immune cells in lymph nodes) are showing strong results in trials. Mirikizumab achieved endoscopic improvement in 40% of patients - meaning visible healing of the gut lining. Ozanimod, already approved for multiple sclerosis, is being tested for Crohn’s and could offer a convenient oral option. Biosimilars are expanding access. In 2023, the FDA released new guidance making it easier for pharmacies to substitute biosimilars without a doctor’s approval - a big step toward lowering costs. But the biggest change? Starting biologics earlier. In the past, doctors waited until other treatments failed. Now, experts recommend starting biologics right away if you have deep ulcers, fistulas, or a family history of surgery. One study showed this approach cut the risk of needing surgery by 50% within five years.What You Can Do
If you’re on a biologic:- Keep track of symptoms with an app like MyIBDCoach - 45% of users say it helps spot flares early.
- Ask about therapeutic drug monitoring. Don’t assume your doctor is doing it - request it.
- Know your insurance coverage. Ask about patient assistance programs - many drugmakers cover 30-50% of out-of-pocket costs.
- Get vaccinated. Flu, pneumonia, and shingles shots are safe and important. Avoid live vaccines like yellow fever.
- Don’t stop without talking to your doctor. Even if you feel fine, stopping can trigger a severe flare.
Can biologic therapy cure Crohn’s disease?
No, biologic therapy cannot cure Crohn’s disease. It doesn’t remove the underlying genetic or immune triggers. But it can put the disease into deep remission, heal intestinal damage, prevent complications like strictures and fistulas, and significantly reduce the need for surgery. Many people live symptom-free for years while on biologics, but stopping treatment often leads to a return of inflammation.
How long does it take for biologics to work?
It varies by drug. Anti-TNF agents like infliximab and adalimumab often start working in 2 to 4 weeks, with noticeable symptom relief within a few months. Vedolizumab takes longer - most people see improvement after 10 to 14 weeks. Ustekinumab can show results in as little as 8 weeks. Full mucosal healing may take 6 to 12 months. Patience is key, but if there’s no change after 12 weeks, your doctor may adjust your treatment.
Are biosimilars as effective as brand-name biologics?
Yes. Biosimilars like Inflectra (infliximab-dyyb) are highly similar to their brand-name counterparts in structure, function, and clinical effect. The FDA requires them to show no meaningful differences in safety or effectiveness. Studies show they work just as well for inducing and maintaining remission in Crohn’s disease. Many patients switch successfully without losing control of their symptoms.
Can I get vaccinated while on biologics?
Yes - but only certain vaccines. Inactivated vaccines like flu, pneumonia, hepatitis B, and shingles (Shingrix) are safe and recommended. Live vaccines - such as MMR, varicella, or nasal flu - are not safe because they contain weakened viruses that could cause infection in someone with a suppressed immune system. Always check with your gastroenterologist before getting any shot.
What happens if a biologic stops working?
This is called loss of response, and it’s common - especially with anti-TNF drugs. It can happen because your body builds antibodies against the drug or because your inflammation becomes more aggressive. The solution isn’t always switching drugs. Your doctor may first check your drug levels and antibody levels. If levels are low, they might increase the dose or shorten the interval. If antibodies are high, switching to a different class - like vedolizumab or ustekinumab - is often the next step.
Do biologics increase cancer risk?
There’s a small increased risk of certain skin cancers and lymphoma, but the overall risk remains low. The biggest cancer concern is skin cancer - regular skin checks are advised. The risk of lymphoma is about 1 in 1,000 patients per year, which is slightly higher than the general population but still rare. The benefits of controlling severe Crohn’s - which itself increases cancer risk - usually outweigh this small risk. Your doctor will monitor you closely and weigh the pros and cons.
ryan Sifontes
January 28, 2026 AT 14:59Laura Arnal
January 29, 2026 AT 08:12Jasneet Minhas
January 31, 2026 AT 05:15Eli In
January 31, 2026 AT 23:28Megan Brooks
February 2, 2026 AT 15:38Ryan Pagan
February 3, 2026 AT 19:23Paul Adler
February 4, 2026 AT 09:32Robin Keith
February 6, 2026 AT 07:23Sheryl Dhlamini
February 7, 2026 AT 16:39Doug Gray
February 9, 2026 AT 10:28Kristie Horst
February 9, 2026 AT 15:13LOUIS YOUANES
February 10, 2026 AT 10:50