When you take a pill, you expect it to work the way it should. But what if your morning grapefruit juice, your daily fish oil, or that herbal tea you drink to relax is quietly messing with your medicine? Drug interactions aren’t rare oddities-they’re common, dangerous, and often invisible. Millions of people take prescription drugs every day, and nearly half also use supplements or follow diets that can turn safe medications into risks. This isn’t just about side effects. It’s about heart attacks, kidney failure, blood clots, and even death-all preventable if you know what to watch for.
How Drug Interactions Actually Work
Not all interactions are the same. They fall into two main buckets: pharmacodynamic and pharmacokinetic. Pharmacodynamic means two substances act on the same part of your body, either doubling up or canceling each other out. For example, if you’re on a blood thinner like warfarin and take ginkgo biloba, both thin the blood. Together, they can push you into dangerous bleeding territory. On the flip side, if you take St. John’s wort while on an antidepressant, the supplement can block the drug’s effect entirely-leaving your depression untreated. Pharmacokinetic interactions are sneakier. They change how your body absorbs, breaks down, or gets rid of a drug. The liver is the main player here, using enzymes like CYP3A4 to process hundreds of medications. Some foods and supplements can shut down these enzymes or turn them into overdrive. Grapefruit juice is the classic example: it shuts down CYP3A4 in your gut, so your body absorbs way more of the drug than intended. One glass of grapefruit juice can make simvastatin-used to lower cholesterol-up to 15 times more potent. That spike raises your risk of rhabdomyolysis, a condition where muscle tissue breaks down and clogs your kidneys. It’s rare, but when it happens, it’s life-threatening.Foods That Fight Your Medicine
You wouldn’t think a banana or a spinach salad could interfere with your heart medication, but they can. Here’s what to watch for:- Grapefruit and citrus fruits: Not just grapefruit-Seville oranges, pomelos, and even some limes can block CYP3A4. This affects statins (like simvastatin and atorvastatin), blood pressure meds (like felodipine), and even some anti-anxiety drugs. One study found that just one 8-ounce glass of grapefruit juice could keep the enzyme blocked for over 24 hours.
- Vitamin K-rich foods: Spinach, kale, broccoli, Brussels sprouts, and green tea are packed with vitamin K. If you’re on warfarin, this vitamin directly counteracts the drug’s blood-thinning effect. A 2018 study showed that eating 150g of cooked spinach in one day could slash warfarin’s effectiveness by 30-40%. The fix? Don’t cut these foods out. Just keep your intake steady. Eat the same amount every day so your dose can adjust accordingly.
- Cranberry juice: Despite popular myths, cranberry juice doesn’t help with UTIs in most cases. But it does interact dangerously with warfarin. At least 28 cases have been documented where cranberry juice pushed INR levels above 8.0 (normal is 2.0-3.0), leading to uncontrolled bleeding. Even small amounts can add up over time.
- Dairy and calcium: Antibiotics like tetracycline and ciprofloxacin bind to calcium, magnesium, and iron in milk or supplements, making them useless. Take them at least two hours before or after dairy.
- Alcohol: Mixing alcohol with painkillers, sedatives, or antidepressants can slow your breathing, crash your blood pressure, or overload your liver. Even moderate drinking with acetaminophen can cause liver damage over time.
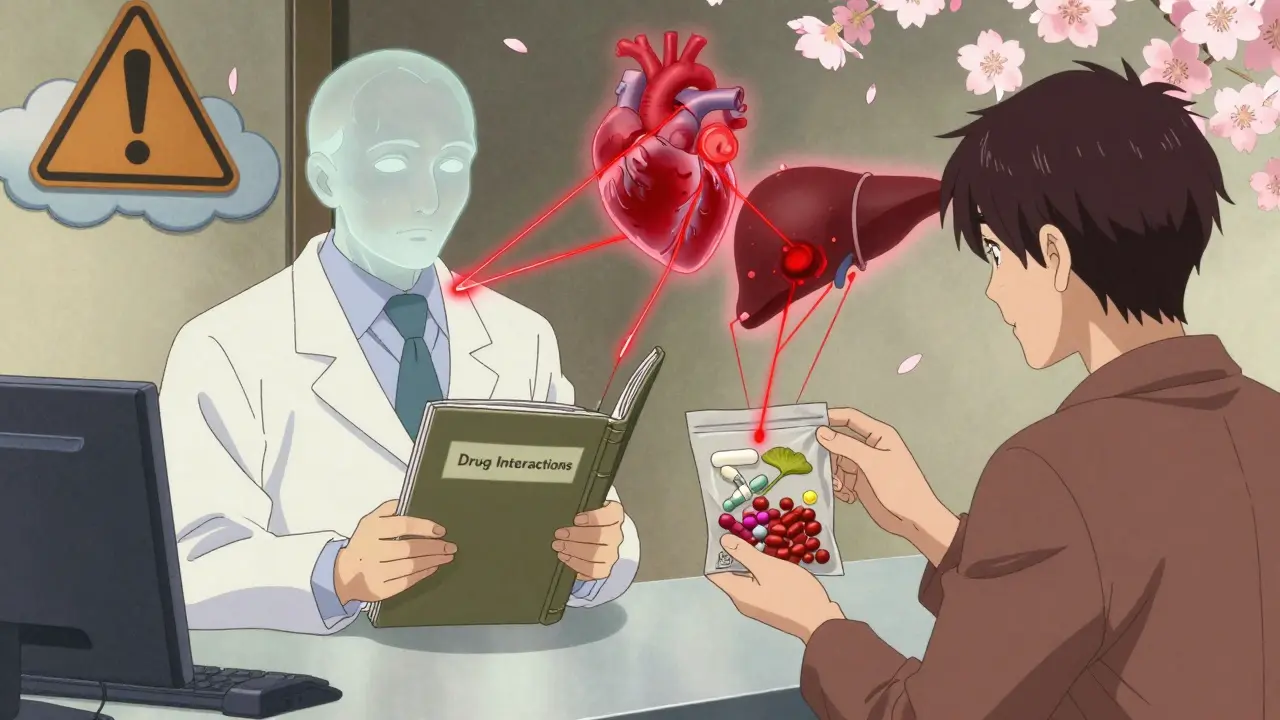
Supplements That Can Be Dangerous
The supplement industry is booming. In 2023, over 70% of U.S. adults took at least one supplement. But unlike prescription drugs, supplements don’t need to prove safety or effectiveness before hitting shelves. And their interactions? Often ignored.- St. John’s wort: This herb, often used for mild depression, is one of the most dangerous supplements on the market. It activates CYP3A4 enzymes so aggressively that it can reduce blood levels of cyclosporine (a transplant drug) by 70%, birth control pills by 50%, and HIV medications by up to 80%. The result? Organ rejection, unplanned pregnancy, or drug-resistant HIV. It’s not a harmless herbal remedy-it’s a pharmacological wrecking ball.
- Ginkgo biloba: Used for memory and circulation, ginkgo thins the blood by inhibiting platelet aggregation. When combined with aspirin, warfarin, or even NSAIDs like ibuprofen, it can lead to brain bleeds or prolonged bleeding after surgery. Studies show it can increase bleeding time by 30-50%.
- Garlic supplements: Garlic in food is fine. But concentrated garlic pills? They have the same blood-thinning effect as aspirin. At least 32 case reports link garlic supplements to excessive bleeding when taken with anticoagulants.
- Red yeast rice: Sold as a natural cholesterol-lowering aid, it contains monacolin K-the same active ingredient as the statin drug lovastatin. Taking it with a prescription statin is like doubling your dose. That raises your risk of muscle damage (myopathy) by over 2 times, according to a 2017 study.
- Coenzyme Q10: Often taken for energy or heart health, CoQ10 may reduce the effectiveness of statins. It’s not a full cancellation, but enough to make your cholesterol numbers worse than before.
Why You’re Not Telling Your Doctor
Here’s the biggest problem: most people don’t tell their doctors about supplements. A 2022 editorial in JAMA Internal Medicine found that 70% of patients who take herbal products never mention them during appointments. Why? They think supplements are “natural,” so they’re safe. Or they assume their doctor doesn’t care. Or they’re embarrassed. But doctors need to know everything. A pharmacist in Bristol told me about a 68-year-old man who came in with severe muscle pain. He was on simvastatin and had started taking red yeast rice “to feel better.” He didn’t realize he was essentially taking two statins. His creatine kinase levels were through the roof-he needed hospitalization. He had no idea his “natural remedy” was the cause. The same goes for food. Patients often say, “I eat a healthy diet,” but don’t realize that their daily kale smoothie is sabotaging their warfarin. Doctors can’t help if they don’t know what’s happening.
How to Stay Safe
You don’t have to give up your supplements or your diet. You just need a plan.- Make a full list: Write down every pill, capsule, tea, and powder you take-even the ones you only use once a week. Include OTC meds like ibuprofen or antacids. Update it every time you see a doctor or pharmacist.
- Bring it to every appointment: Don’t rely on memory. Show the list. Ask: “Could any of these interact with my prescriptions?”
- Use trusted tools: The FDA’s online drug interaction checker and MedlinePlus are free and reliable. The LiverTox database from the NIH has detailed, evidence-based info on 1,200+ supplement-drug combos.
- Ask your pharmacist: Pharmacists are trained to catch interactions. A 2022 study found that pharmacist-led reviews cut adverse events by 22%. They’re often more accessible than your doctor.
- Be consistent: If you’re on warfarin, eat the same amount of vitamin K every day. Don’t go from spinach salads every day to none for a week. Stability matters more than perfection.
What’s Changing
There’s hope. The FDA is pushing for stricter labeling on supplements. A 2023 draft guidance now requires new drugs to be tested for interactions with common supplements like St. John’s wort and ginkgo. The National Institutes of Health has poured $15.7 million into research on these interactions. And AI tools are being trained to scan clinical notes and flag hidden risks-IBM Watson’s pilot system predicted novel interactions with 87% accuracy. But the biggest change needs to come from you. Talk. Ask. Share. Don’t assume. Your medicine works best when your whole health picture is clear.Can I still drink grapefruit juice if I’m on medication?
It depends on the drug. Grapefruit juice can dangerously increase levels of statins (like simvastatin), some blood pressure meds (like felodipine), and certain anti-anxiety drugs. If you’re on any prescription medication, check with your pharmacist before drinking grapefruit juice. Even small amounts can have lasting effects-up to 24 hours. If in doubt, avoid it entirely.
Are herbal supplements safer than prescription drugs?
No. Just because something is labeled “natural” doesn’t mean it’s safe. St. John’s wort, ginkgo, and garlic supplements have been linked to life-threatening interactions. Unlike prescription drugs, supplements aren’t required to prove they’re safe or effective before being sold. Many have potent effects on your liver, blood, or heart-sometimes stronger than over-the-counter painkillers.
I take fish oil. Is that risky?
Fish oil can thin your blood, especially in high doses (over 3 grams daily). If you’re on warfarin, aspirin, or clopidogrel, combining it with fish oil increases bleeding risk. Talk to your doctor about your dose. For most people on low doses (under 1 gram), it’s fine-but always disclose it on your medication list.
What should I do if I think I’m having a drug interaction?
Stop the supplement or food causing the issue, if possible, and contact your doctor or pharmacist immediately. Signs include unusual bruising, muscle pain or weakness, dizziness, confusion, chest pain, or sudden changes in how you feel. Don’t wait. Some interactions can escalate quickly-especially with blood thinners or heart medications.
Can I use online interaction checkers instead of talking to a doctor?
Online tools like MedlinePlus or the FDA’s checker are great for initial checks-but they’re not a replacement for professional advice. They don’t know your full medical history, your dosage, or how your body responds. Use them as a starting point, then always confirm with a pharmacist or doctor. They can spot patterns an algorithm might miss.

James Roberts
February 18, 2026 AT 22:05Thanks for the heads-up. I’m switching to orange juice. Or maybe just water. Or maybe I’ll just start drinking whiskey instead. At least I know what’s in that.