MAOI Medication Safety Checker
Medication Checker
Safety Results
Results will appear here after checking medications
Important Washout Period
Imagine taking a common cold medicine-something you’ve used dozens of times-only to have your blood pressure spike so fast your head feels like it’s going to explode. That’s not a horror story. It’s a real, documented danger when ephedrine meets MAO inhibitors. This isn’t a rare edge case. It’s a lethal interaction that has killed people, caused strokes, and sent others to the ER with brain bleeds-all from a single pill.
What Happens When Ephedrine Meets an MAOI?
Ephedrine is a stimulant. It’s found in some cold and allergy meds, weight loss supplements, and even energy drinks. It works by forcing your body to release norepinephrine-the same chemical your brain uses to ramp up heart rate, tighten blood vessels, and raise blood pressure. That’s why it helps clear a stuffy nose. But if you’re taking an MAOI, your body can’t break down that extra norepinephrine. Ever. MAOIs, or monoamine oxidase inhibitors, are antidepressants. They’re powerful. They work by blocking the enzyme that normally clears out excess neurotransmitters like norepinephrine, serotonin, and dopamine. That’s good for depression. But when ephedrine floods your system with more of these chemicals, and the MAOI won’t let them leave? The result is a runaway surge. Blood pressure can hit 200 mmHg or higher in under an hour. That’s like driving your car at 150 mph with no brakes.It’s Not Just One Pill-It’s a Silent Bomb
You don’t need to take a lot. A single 25 mg dose of ephedrine-half the amount in some OTC decongestants-is enough to trigger a crisis if you’re on an MAOI. That’s why so many cases start with someone thinking, “It’s just a cold pill. I’ve taken it before.” The first signs aren’t subtle. You’ll feel a crushing headache, usually starting at the back of your skull and shooting forward. Your heart pounds. Your vision blurs. You sweat like you’ve run a marathon in freezing weather. Nausea, vomiting, stiff neck, dilated pupils-these aren’t side effects. They’re warning signs your body is under siege. In extreme cases, the pressure ruptures blood vessels in the brain, causing a subarachnoid hemorrhage. That’s what happened in the 1965 case that first put this interaction on the map. A woman took ephedrine while on an MAOI. Within 30 minutes, she lost consciousness. A CT scan showed bleeding in her brain. She didn’t survive.Which MAOIs Are the Most Dangerous?
Not all MAOIs are created equal. The older, irreversible ones are the real killers: phenelzine (Nardil), tranylcypromine (Parnate), isocarboxazid (Marplan), and nialamide. These bind to the enzyme permanently. It takes two to three weeks for your body to make new enzymes after you stop taking them. That means even if you quit your MAOI last week, you’re still at risk. Even newer options aren’t safe. Selegiline (Emsam) comes as a patch. At low doses (6 mg/24hr), it mostly targets MAO-B, which is linked to dopamine. But at higher doses, it hits MAO-A-the one that clears norepinephrine. That’s when the danger returns. And even if you’re on a reversible MAOI like moclobemide, you’re not safe. You just need a bigger dose of ephedrine to trigger the crisis. And most cold pills contain way more than that.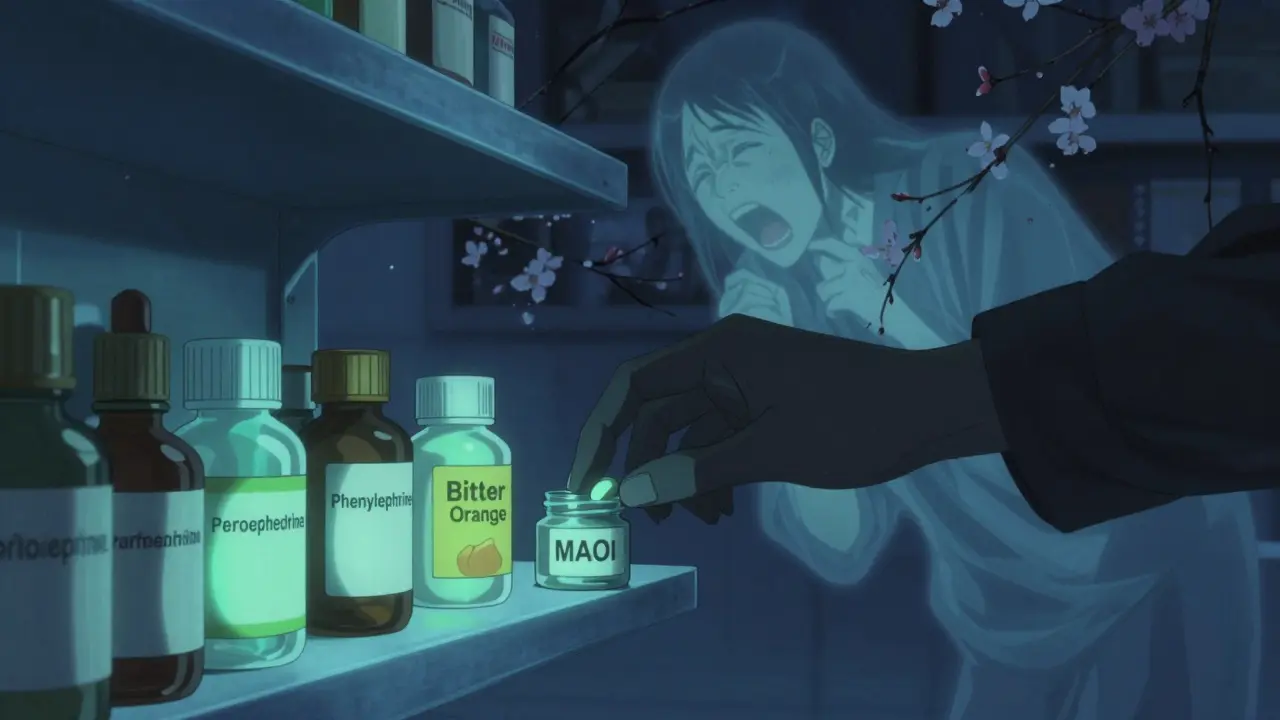
What’s in Your Medicine Cabinet?
Ephedrine isn’t the only culprit. Pseudoephedrine, phenylephrine, and phenylpropanolamine-all common in cold and allergy meds-do the same thing. So do certain weight loss pills, energy boosters, and even some herbal supplements like bitter orange or yohimbine. If a product says “decongestant,” “stimulant,” or “appetite suppressant,” it’s a red flag. The FDA has issued black box warnings-the strongest possible-for all MAOIs because of this interaction. Yet, every year, people still end up in the ER because their doctor didn’t warn them, or their pharmacist didn’t flag it, or they didn’t realize their “natural” supplement contained ephedrine-like compounds.What If You’ve Already Taken Both?
If you’ve accidentally taken ephedrine while on an MAOI, don’t wait. Call 911 or go to the ER immediately. Do not try to treat this at home. Sublingual nifedipine (a blood pressure pill you might think of using) is dangerous-it can drop your pressure too fast and cause a stroke. Emergency treatment requires IV phentolamine, a drug that blocks the effects of excess norepinephrine. Time is critical. The faster you get treatment, the less likely you are to suffer permanent damage. Cases show that delays of even 30 minutes can mean the difference between survival and death.How to Stay Safe
The only guaranteed way to avoid this crisis is to never mix the two. Period.- If you’re on an MAOI, avoid every OTC cold, flu, or allergy medicine unless your psychiatrist or pharmacist has approved it.
- Don’t assume “natural” means safe. Bitter orange, yohimbine, and green tea extract can all trigger the same reaction.
- Wait at least 14 days after stopping an irreversible MAOI before taking any stimulant, even if you feel fine.
- For reversible MAOIs like moclobemide, wait 48 hours-but still check with your doctor.
- Carry an MAOI alert card. The Mayo Clinic found that 87% of patients who did this avoided accidental exposure.

Why Is This Still Happening?
MAOIs are rare now-less than 1% of antidepressant prescriptions in the U.S. But they’re not gone. They’re the last resort for people who haven’t responded to anything else. For some, they’re the only thing that lifts the fog of depression. The problem? Most doctors outside of psychiatry don’t know the risks. A 2021 study in JAMA Internal Medicine found that 22% of people prescribed MAOIs still got at least one contraindicated drug within 30 days-often from their primary care provider or dentist. Pharmacies don’t always flag it. Online pharmacies don’t screen at all. Reddit threads from people on MAOIs are full of stories: “I took Sudafed and thought I was having a panic attack-turns out my blood pressure was 240.” “My vision went white. I thought I was dying.” “I didn’t know MAOIs meant no cold medicine.”The Future: Safer Options?
There’s hope. In March 2023, the FDA approved befloxatone, a new reversible MAOI with a 6-hour half-life. Early data suggests it’s 90% less likely to cause a hypertensive crisis. It’s not on the market yet, but it’s a sign that researchers are working on safer versions. NIH is also testing wearable patches that monitor blood pressure continuously. The goal? Alert you before a crisis hits. But until those tools are widely available, the only rule that matters is simple: don’t mix them.Bottom Line: This Interaction Is Non-Negotiable
There’s no safe dose. No “maybe.” No “I’ve been fine before.” If you’re on an MAOI, ephedrine and its cousins are off-limits. Always. No exceptions. The risk isn’t theoretical. It’s been proven in hospitals, in coroner’s reports, and in the quiet, terrified voices of people who nearly died because they didn’t know. Your health isn’t worth gambling on. If you’re unsure whether a medication is safe, ask your psychiatrist. Ask your pharmacist. Ask twice. Better safe than dead.Can I take ephedrine if I stopped my MAOI two weeks ago?
Yes, but only if you stopped an irreversible MAOI like phenelzine or tranylcypromine. The standard washout period is 14 days. However, if you’re unsure which MAOI you took or how long it stays in your system, check with your doctor. For reversible MAOIs like moclobemide, 48 hours is enough. Never assume-confirm with your prescriber.
Are all decongestants dangerous with MAOIs?
Yes. Pseudoephedrine, phenylephrine, phenylpropanolamine, and ephedrine all act as sympathomimetics and carry the same risk. Even “natural” decongestants like bitter orange or yohimbine can trigger a crisis. Always read labels and ask your pharmacist before taking anything for congestion, allergies, or weight loss.
What should I do if I experience symptoms after taking ephedrine?
Call 911 or go to the nearest emergency room immediately. Do not wait. Symptoms like severe headache, chest pain, blurred vision, nausea, or rapid heartbeat are signs of a hypertensive crisis. Do not take any blood pressure pills at home-especially nifedipine. Only IV phentolamine in a hospital setting is safe and effective.
Is this interaction only a problem with antidepressants?
No. MAOIs are used for depression, but also for Parkinson’s, anxiety, and sometimes chronic pain. Any medication that inhibits monoamine oxidase-whether prescribed for mental health or neurological conditions-carries this risk. Always disclose all medications you’re taking, including supplements.
Why aren’t MAOIs banned if they’re so dangerous?
Because they work when nothing else does. For people with treatment-resistant depression-especially those with atypical symptoms like oversleeping and overeating-MAOIs can be life-changing. The risk is real, but so is the benefit. That’s why they’re still used, but only under strict supervision. The goal isn’t to eliminate them-it’s to make sure no one takes them without knowing the risks.

pragya mishra
January 20, 2026 AT 09:08This is why people die from OTC meds. I work in a pharmacy in Mumbai and see this every week-someone takes pseudoephedrine with their antidepressant and thinks they’re fine. No one reads labels. No one asks. And then they end up in the ER with a stroke. It’s not complicated. It’s negligence.
Manoj Kumar Billigunta
January 21, 2026 AT 01:41Hey, I’m a med student in Hyderabad. Just wanted to add-MAOIs aren’t the only thing you need to watch. Even some herbal teas like St. John’s Wort or high-dose green tea extract can interact. I’ve seen patients come in with BP spikes after drinking ‘natural energy tonics’ from the market. Always check with your pharmacist. Even if it says ‘herbal’ or ‘organic,’ it’s not magic. It’s chemistry.
Andy Thompson
January 22, 2026 AT 21:45LOL. The FDA is just trying to control us. They banned ephedrine in 2004 but now they want us to believe it’s safe if you wait 14 days? That’s a lie. Big Pharma doesn’t want you to know that natural stimulants work better than their $500/month antidepressants. They’re scared people will stop taking SSRIs and go back to ephedrine. This whole thing is a scam to keep you hooked on pills.
Also, I saw a video on Telegram where a guy took Sudafed and his eyes turned red and he started screaming. They said it was a ‘hypertensive crisis’ but I think it was the government’s mind control beam. They’re testing it on MAOI users.
Art Gar
January 24, 2026 AT 09:15It is imperative to underscore that the pharmacological interaction between monoamine oxidase inhibitors and sympathomimetic agents constitutes a well-documented, life-threatening contraindication. The persistence of this clinical hazard, despite decades of published literature and explicit black-box warnings, reflects a systemic failure in patient education and interprofessional communication. One cannot overstate the gravity of this issue.
Edith Brederode
January 25, 2026 AT 00:42Thank you for writing this. 🙏 I’m on phenelzine and I used to take NyQuil like it was candy. I had no idea. This literally saved my life. I’m sharing this with my entire family now. Please, if you’re on an MAOI-don’t wing it. Ask. Twice.
Crystal August
January 25, 2026 AT 23:50You people are so dramatic. I’ve been on Parnate for 8 years and I took Sudafed last winter. Felt a little jittery, sure, but I’m fine. If you’re scared of medicine, maybe you shouldn’t be taking anything at all. This is fearmongering wrapped in a medical article.
sagar sanadi
January 26, 2026 AT 18:30So let me get this straight… you’re telling me I can’t take a cold pill because some doctor says so? What if I just take half? Or wait 12 hours? Or maybe I’ll just drink a bunch of water and pray? Come on. This is why America is falling apart-too many rules, not enough common sense.
Nadia Watson
January 28, 2026 AT 17:34As someone who’s worked in global health for 15 years, I’ve seen this exact interaction kill people in rural India and inner-city Detroit alike. The real tragedy isn’t the drug combo-it’s that so many patients aren’t given proper counseling. In places without access to psychiatrists, people are left to guess. This post should be printed and handed out with every MAOI prescription. Not just posted online.
Also, typo: ‘nialamide’ should be ‘nisentamide’? No, wait-nialamide is correct. My bad. Anyway.
Courtney Carra
January 29, 2026 AT 10:19It’s funny how we treat medicine like it’s a moral test. ‘Don’t mix them. Never.’ But life isn’t binary. What if you’re in a foreign country and your headache is unbearable? What if your pharmacist doesn’t speak English? What if you’re depressed and desperate and you just want to breathe? The answer isn’t fear. It’s education. It’s access. It’s compassion. We’re not robots. We’re humans trying to survive in a system that treats us like liabilities.
Renee Stringer
January 31, 2026 AT 04:13People need to stop treating their bodies like they’re playing a video game. You don’t get a ‘retry’ after a brain bleed.