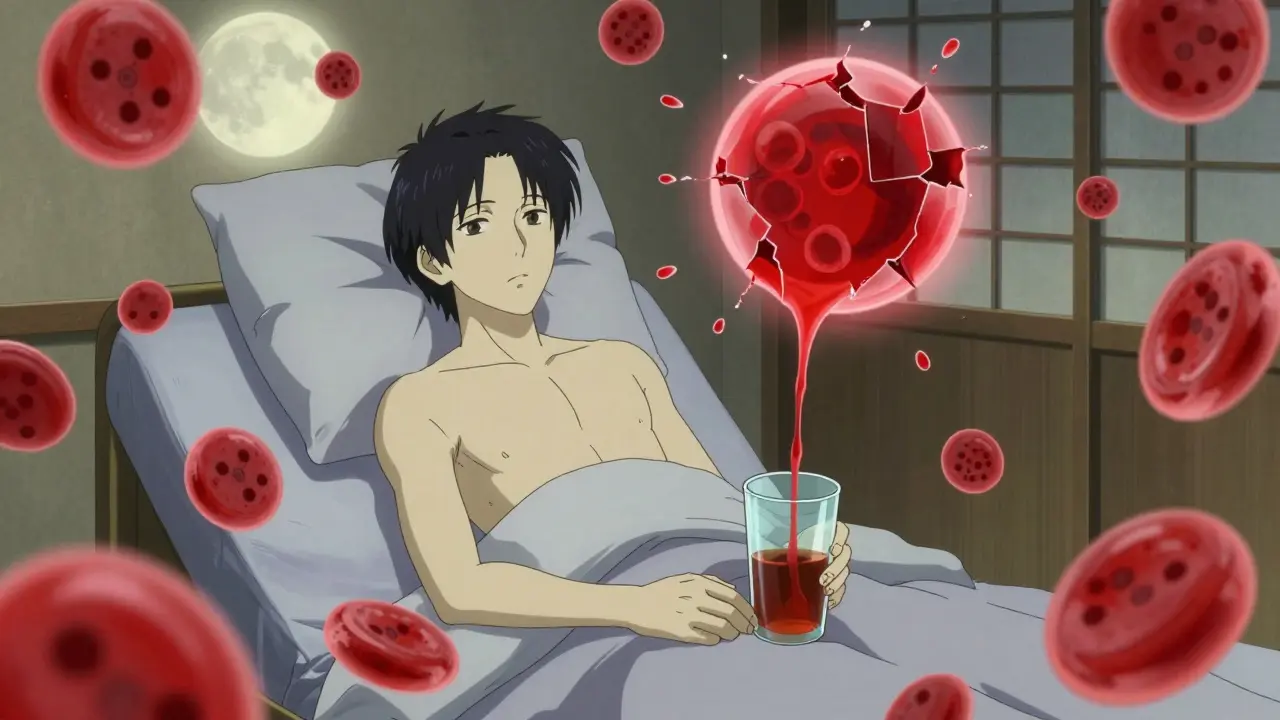
When a medicine you’re taking starts attacking your own red blood cells, it’s not just a side effect-it’s a medical emergency. Drug-induced hemolytic anemia is rare, but when it happens, it can turn a routine prescription into a life-threatening situation. This isn’t about mild nausea or dizziness. This is about your body’s immune system or your blood’s chemistry suddenly turning on the very cells that carry oxygen to every organ, every muscle, every breath you take.
How a Medicine Can Destroy Your Red Blood Cells
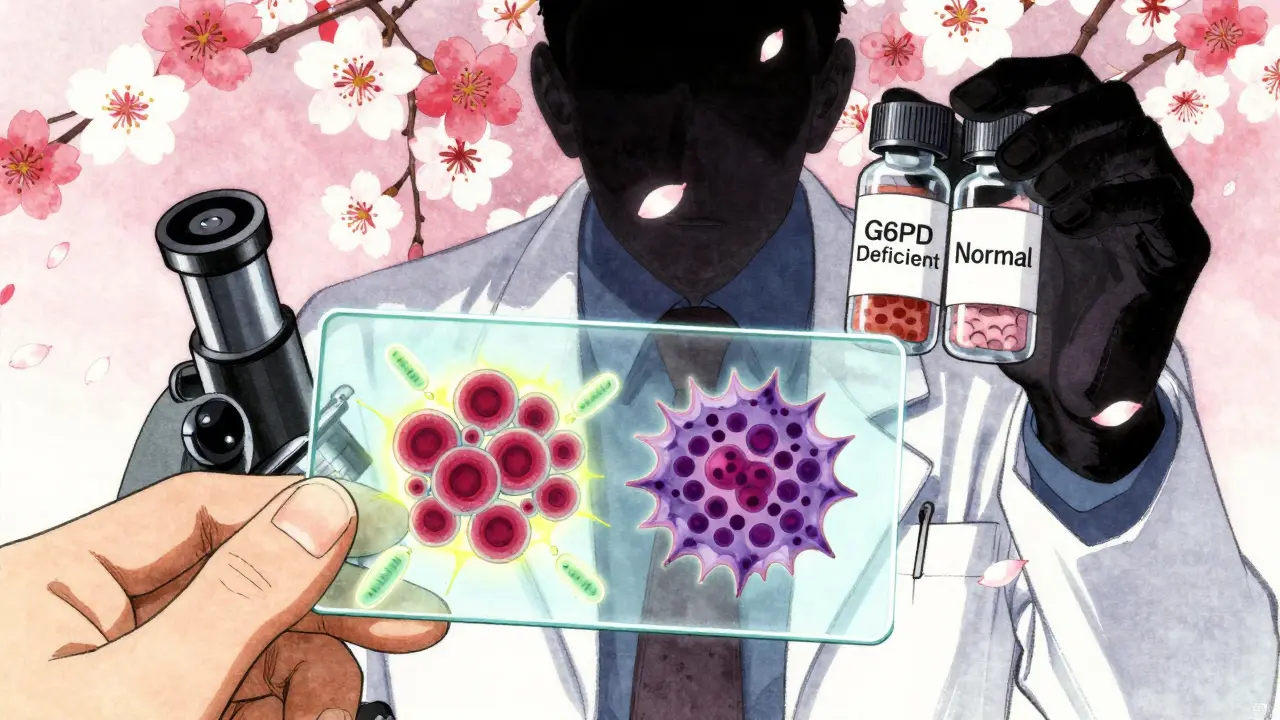
Your red blood cells normally live for about 120 days. They’re made in your bone marrow, cruise through your veins, deliver oxygen, and then get quietly recycled. But with drug-induced hemolytic anemia, that lifespan can shrink to hours or days. There are two main ways this happens. The first is immune-mediated. Some drugs, especially certain antibiotics, stick to the surface of your red blood cells like sticky notes. Your immune system sees these drug-coated cells as foreign invaders and sends antibodies to destroy them. Think of it like your body mistaking your own car for a stolen vehicle because someone painted a fake license plate on it. The most common culprits? Cephalosporin antibiotics-especially cefotetan, ceftriaxone, and piperacillin. Together, they cause about 70% of all immune-mediated cases. The second mechanism is oxidative damage. Here, the drug doesn’t trigger an immune response. Instead, it overwhelms your red blood cells’ natural defenses. If you have a genetic condition called G6PD deficiency-common in 10-14% of African American men and 4-15% of people with Mediterranean ancestry-your cells can’t handle certain oxidants. Even normal doses of drugs like dapsone, phenazopyridine (Pyridium), or nitrofurantoin can cause these cells to break apart. The result? Heinz bodies, which are clumps of damaged hemoglobin that shred the cell from the inside. And here’s the catch: you might not know you have G6PD deficiency until a drug triggers a crisis. It’s silent until it’s not.Which Medications Are Most Likely to Cause This?
Not every drug causes this. But a small group has been linked to hemolytic anemia over and over again. The list isn’t long, but the consequences are serious. For immune-mediated cases:- Cefotetan
- Ceftriaxone
- Piperacillin
- Methyldopa (less common now, but historically significant)
- Penicillin and related antibiotics
- Some NSAIDs like ibuprofen or naproxen in rare cases
- Dapsone
- Phenazopyridine (Pyridium)
- Nitrofurantoin
- Primaquine
- Sulfa drugs
- Topical benzocaine (used in throat sprays or dental gels)
- Amyl nitrate, butyl nitrate (sometimes used recreationally or for angina)
- Ribavirin
What Does It Feel Like? The Symptoms You Can’t Ignore
The symptoms of drug-induced hemolytic anemia don’t come on slowly. They hit fast and hard. Fatigue? Yes. But it’s not just being tired. It’s collapsing after walking to the kitchen. Shortness of breath? Not from climbing stairs-just from sitting up in bed. Here’s what patients actually report:- Extreme fatigue (92% of cases)
- Weakness so severe it feels like your limbs are made of lead (87%)
- Shortness of breath at rest (76%)
- Heart racing even when lying down (68% with heart rate over 100 bpm)
- Pale skin, almost grayish (73%)
- Yellow eyes and skin (jaundice, 81%)
- Dark, tea-colored urine (from hemoglobin breaking down)
How Doctors Diagnose It (And Why It’s Often Missed)
This condition is misdiagnosed in nearly half of cases. Why? Because the symptoms look like every other kind of anemia-or worse, like the flu. The key is knowing what tests to run. Here’s the diagnostic checklist:- Low hemoglobin-obviously. But how fast did it drop? A sudden drop over days points to hemolysis, not slow production.
- High indirect bilirubin-above 3 mg/dL. This comes from broken-down hemoglobin.
- High LDH-above 250 U/L. This enzyme leaks out of destroyed red blood cells.
- Low haptoglobin-below 25 mg/dL. Haptoglobin binds free hemoglobin, so it gets used up fast during hemolysis.
- Peripheral smear-looking at blood under a microscope. Spherocytes (small, round red cells) mean immune destruction. Heinz bodies (clumps inside cells) mean oxidative damage.
- Direct antiglobulin test (DAT)-positive in 95% of immune cases. But it can be negative early on or with certain drugs.
- G6PD enzyme test-but don’t test during active hemolysis. The test will be falsely normal because new red blood cells (reticulocytes) still have enzyme activity. Wait 2-3 months after recovery.
What Happens When You Stop the Drug?
The single most important thing you can do? Stop taking the medicine. That’s it. That’s the first and most effective treatment. In 95% of cases, hemolysis stops within days of discontinuation. Hemoglobin levels begin to recover in 7-10 days. Full recovery usually takes 4-6 weeks. But stopping the drug isn’t always enough. If hemoglobin falls below 7-8 g/dL, you’ll need a blood transfusion. Not because it’s a cure-but because your body is starving for oxygen. Without it, your heart can’t keep up. Steroids like prednisone are sometimes used, but their benefit is unclear. Many patients recover just fine without them. The real problem comes when the immune system keeps attacking even after the drug is gone. That’s called drug-independent autoantibodies. In those cases, you need stronger treatments:- Intravenous immunoglobulin (IVIG)-1 gram per kilogram for two days
- Rituximab-a monoclonal antibody given weekly for four weeks
- Azathioprine or cyclosporine-long-term immunosuppressants
What About Methylene Blue? It Can Kill You
If you develop methemoglobinemia-a condition where iron in hemoglobin gets stuck in the wrong form-you might be given methylene blue. It’s a life-saving drug in severe cases (when methemoglobin levels exceed 30%). But if you have G6PD deficiency? Don’t even think about it. Methylene blue can trigger massive hemolysis. It’s not just risky-it’s deadly. The American Academy of Family Physicians explicitly warns against it in G6PD-deficient patients. That’s why knowing your G6PD status matters-not just for antibiotics, but for every drug you’re given.
Why This Matters More Than You Think
This isn’t just a rare textbook case. It’s happening right now in hospitals and clinics. A 2023 study showed that 34% of severe DIIHA cases led to dangerous blood clots-venous thromboembolism. Your body goes into a hypercoagulable state after massive red blood cell destruction. So even if your hemoglobin is low, you still need blood thinners to prevent clots. And children? It’s rare in kids-but when it happens, it’s worse. A 2023 pediatric study found children presented with an average hemoglobin of 5.2 g/dL, compared to 6.8 g/dL in adults. They’re more vulnerable. Hospitals that added automated alerts in their electronic health records for high-risk drugs saw a 32% drop in severe cases over 18 months. That’s not magic. That’s awareness.What You Should Do If You’re on These Medications
If you’re taking any of the drugs listed above-especially cephalosporins, dapsone, or phenazopyridine-and you start feeling unusually tired, short of breath, or notice your skin or eyes turning yellow:- Stop the medication immediately.
- Call your doctor or go to urgent care.
- Ask: “Could this be drug-induced hemolytic anemia?”
- Insist on the basic tests: hemoglobin, LDH, haptoglobin, bilirubin, and a blood smear.
- If you’re of African, Mediterranean, or Southeast Asian descent, ask about G6PD deficiency testing-after the episode has passed.
Looking Ahead: What’s Changing in Diagnosis and Treatment
New tools are emerging. Clinical trials are testing drugs like efgartigimod (NCT05678901), which clears harmful antibodies from the blood. Early results show a 67% response rate in just four weeks. Complement inhibitors (NCT05812345) are also being studied for severe cases. But the biggest change isn’t a new drug-it’s awareness. More doctors are learning the red flags. More labs are tracking patterns. More hospitals are building alerts into their systems. The goal isn’t just to treat it. It’s to prevent it before it starts.Can a single dose of a medication cause hemolytic anemia?
Yes, especially in people with G6PD deficiency. Drugs like phenazopyridine or dapsone can trigger rapid hemolysis within 24-72 hours after just one dose. Immune-mediated cases usually take longer-7-10 days of continuous use-but oxidative damage can strike fast.
Is hemolytic anemia from drugs common?
No, it’s rare-accounting for less than 1% of all anemia cases. But it’s serious. Because it’s rare, many doctors don’t think of it right away, which delays diagnosis. That’s why awareness matters more than frequency.
Can I get tested for G6PD deficiency before taking a risky drug?
Yes, and you should if you’re of African, Mediterranean, Middle Eastern, or Southeast Asian descent. Testing is simple-a blood test. But don’t test during active hemolysis; results can be falsely normal. Wait 2-3 months after recovery for accurate results.
Will I need a blood transfusion if I get drug-induced hemolytic anemia?
Not always. If your hemoglobin stays above 7-8 g/dL and you’re not severely symptomatic, your body can recover on its own after stopping the drug. But if you’re dizzy, short of breath, or your heart is racing, a transfusion may be needed to prevent heart damage.
Can I ever take the drug again if I had this reaction?
Absolutely not. Once you’ve had drug-induced hemolytic anemia from a specific medication, you must avoid it for life. Re-exposure-even a tiny dose-can trigger an even more severe reaction. Make sure your medical records and pharmacy profile reflect this.
How long does recovery take after stopping the drug?
Most people start improving within 7-10 days. Hemoglobin levels usually return to normal in 4-6 weeks. Full recovery means your bone marrow has rebuilt your red blood cell supply and your immune system has reset. Follow-up blood tests are important to confirm this.
Harriot Rockey
February 5, 2026 AT 03:02Samuel Bradway
February 6, 2026 AT 22:18pradnya paramita
February 7, 2026 AT 07:46Roshan Gudhe
February 8, 2026 AT 12:37Rachel Kipps
February 9, 2026 AT 04:24Ed Mackey
February 11, 2026 AT 01:41Alex LaVey
February 12, 2026 AT 23:47caroline hernandez
February 14, 2026 AT 07:20Jhoantan Moreira
February 14, 2026 AT 16:02Justin Fauth
February 16, 2026 AT 06:46Meenal Khurana
February 17, 2026 AT 21:54Sherman Lee
February 19, 2026 AT 12:58Mandy Vodak-Marotta
February 19, 2026 AT 14:45Alec Stewart Stewart
February 19, 2026 AT 19:17