When two or more drugs are combined into a single pill or formulation, it’s not enough to just match the brand name. Therapeutic equivalence is what determines whether you can safely swap one combination product for another - even if they come from different manufacturers. This isn’t just a technical detail. It’s the difference between a patient staying stable on their medication and ending up in the hospital because a switch didn’t account for subtle differences in how the drugs behave together.
What Therapeutic Equivalence Really Means
Therapeutic equivalence means two drug products - whether brand or generic - contain the same active ingredients, in the same amounts, delivered the same way, and work the same way in the body. The U.S. Food and Drug Administration (FDA) tracks this in the Orange Book, a public database updated monthly. As of 2023, over 14,000 drug products have been rated, and 95% of them carry an ‘A’ rating - meaning they’re considered interchangeable without clinical risk. But here’s the catch: this only applies when everything lines up exactly. Same active ingredients. Same strength. Same dosage form - tablet, capsule, injection. Same route - oral, topical, inhaled. If one product uses a different salt form or has a different release profile, it might be a pharmaceutical alternative, not a therapeutic equivalent. And that’s where things get risky in combination products.Why Combination Products Are Trickier
Combination products - like amlodipine/benazepril for high blood pressure or tramadol/acetaminophen for pain - combine two or more drugs into one. The goal is convenience and better adherence. But when you swap one brand for another, you’re not just swapping one drug. You’re swapping two, and their interaction matters. Take the example of sirolimus and topotecan used in cancer research. One drug reduces cell proliferation by 69.8%, the other by 88.9%. You can’t just assume that swapping one generic version for another will keep the ratio of effect the same. Dose equivalence here isn’t linear. It requires complex modeling using formulas like beq(a)=CBγ(1+CAa)−1, where γ is the efficacy ratio between the two drugs. Even if each component meets bioequivalence standards individually, their combined effect might shift. The FDA’s TE code system helps. An ‘A’ rating means therapeutic equivalence is confirmed. A ‘B’ rating means there’s uncertainty - often because of differences in inactive ingredients, manufacturing processes, or release mechanisms. But even with an ‘A’ rating, problems can arise.The Hidden Risk: Inactive Ingredients and NTI Drugs
Two combination products can have identical active ingredients and still behave differently. Why? Inactive ingredients. Fillers, binders, coatings, and disintegrants can change how quickly the drug is absorbed - especially in narrow therapeutic index (NTI) drugs. NTI drugs have a tiny window between effective and toxic doses. Warfarin, levothyroxine, phenytoin, and digoxin fall into this category. When these are part of a combination, even small changes in absorption can tip the balance. A 2018 study in the Journal of Clinical Endocrinology & Metabolism found that 12% of patients switching between different levothyroxine generics experienced thyroid hormone level shifts - even though all products met FDA’s 80-125% bioequivalence range. For NTI drugs, the FDA requires a tighter bioequivalence range: 90-111%. But that’s still not foolproof. A 2022 report from the FDA Adverse Event Reporting System (FAERS) showed 247 incidents linked to dose conversion errors in combination products. Nearly 40% involved cardiovascular drugs. One pharmacist in Ohio reported three dosing errors in six months just from switching between different generic versions of amlodipine/benazepril. The active ingredients were the same. The strength was the same. But one manufacturer used croscarmellose sodium as a disintegrant; another used sodium starch glycolate. That small difference changed absorption speed - enough to cause dizziness and low blood pressure in elderly patients.
How to Manage Therapeutic Equivalence Safely
Managing therapeutic equivalence in combinations isn’t about guesswork. It’s about systems. The FDA recommends a three-step checklist:- Confirm the active ingredients match exactly - including salt forms and quantities.
- Verify the dosage form and route are identical - no switching from tablet to capsule unless approved.
- Check the Orange Book TE code. Only use products with an ‘A’ rating.
- Train staff for 8-12 weeks on substitution protocols. The University of California Health System cut substitution errors by 65% after a 40-hour training program.
- Use barcode scanning on every combination product. This ensures the exact product and strength are dispensed.
- Implement a 72-hour monitoring window for patients switched on NTI combination drugs. Check labs, watch for side effects, and document changes.
- Keep standardized conversion tables handy - especially for psychiatric and cardiovascular combinations where pharmacokinetics are complex.
Real-World Outcomes: Successes and Failures
Not every switch goes wrong. In fact, most don’t. The generic version of Advair Diskus (fluticasone/salmeterol) achieved 97% therapeutic equivalence to the brand, saving clinics 40% on costs with zero rise in asthma exacerbations. A hospital pharmacy in Minnesota saved $1.2 million a year by switching proton pump inhibitor combinations to generics - with no adverse events reported. But the failures are loud. A nurse practitioner in Texas described a patient who switched from Vytorin (ezetimibe/simvastatin) to a generic equivalent and saw a 15% increase in LDL cholesterol. The active ingredients were identical. The dose was the same. But the generic used a different coating that slowed absorption just enough to reduce effectiveness. These aren’t isolated cases. The Institute for Safe Medication Practices found that 15% of medication errors in 2022 involved incorrect dose conversions between therapeutically equivalent combination products. Many of these happened because prescribers assumed “same strength = same effect,” without considering how the combination as a whole behaves.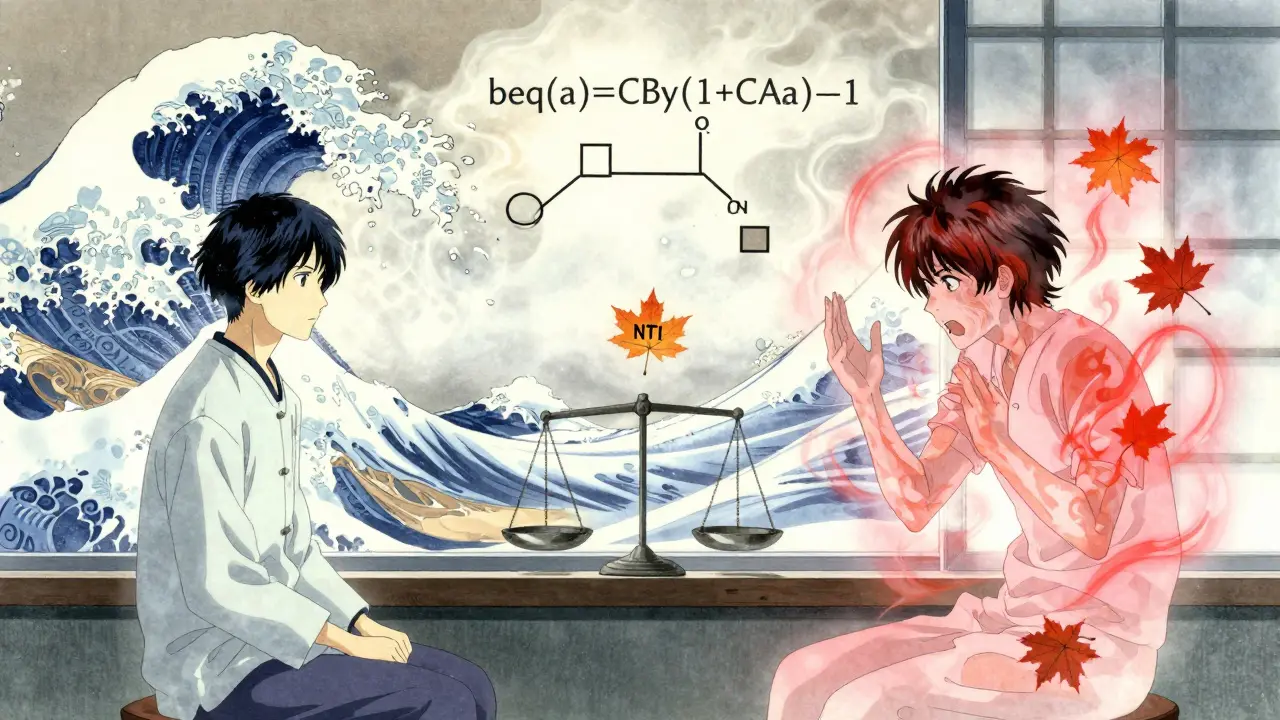
The Future: Personalized Equivalence
The current system was built for a simpler time - when drugs were single agents and patients were treated with averages. Today, we know that people metabolize drugs differently. Genetics, age, liver function, and gut microbiome all affect how a combination works. The FDA is already testing machine learning tools that predict therapeutic inequivalence based on formulation differences. Early results show 89% accuracy in flagging risky substitutions. Meanwhile, the Precision Medicine Initiative predicts that by 2030, 30% of therapeutic equivalence decisions will include pharmacogenomic data - like whether a patient is a slow or fast metabolizer of CYP3A4 enzymes. New proposals are emerging too. One idea: an ‘A*’ rating for combination products that have been proven bioequivalent across multiple strengths - not just one. That would help with dose titration and reduce confusion. But challenges remain. Of the 47 approved combination biologic products as of 2023, only three have established therapeutic equivalence frameworks. Biologics are inherently more complex than small-molecule drugs. Their structure can change slightly with manufacturing - making true equivalence harder to prove.What You Need to Do Now
If you’re a prescriber, pharmacist, or patient:- Don’t assume “generic = interchangeable.” Always check the TE code in the Orange Book.
- For NTI combinations, avoid switching unless absolutely necessary - and monitor closely if you do.
- Use electronic prescribing systems that flag potential substitution risks.
- Ask your pharmacist: “Is this generic version of this combination product rated ‘A’ in the Orange Book?”
- If you’re on a combination drug and feel different after a refill - even slightly - report it. Your experience matters.
Dorine Anthony
December 19, 2025 AT 08:14Been a pharmacist for 12 years and this is the one thing I scream about at staff meetings - just because two pills have the same active ingredients doesn’t mean they feel the same in your body. I had an elderly lady come in crying because her blood pressure went haywire after a switch. Same dose. Same brand name on the label. But the filler was different. She swore it was the same pill. It wasn’t.
People think generics are just cheaper versions. They’re not. They’re different machines with the same engine. And sometimes, the engine sputters.
William Storrs
December 21, 2025 AT 01:41Love this breakdown. Seriously. So many docs just click ‘substitute’ without thinking. This is why we need better training - not just for pharmacists, but for everyone who writes scripts. I’ve started putting ‘DO NOT SUBSTITUTE’ on NTI combos in my EHR. It’s a pain, but it’s saved at least three patients from crashing this year.
Keep pushing this message. The system’s broken, but we can fix it one prescription at a time.
James Stearns
December 22, 2025 AT 12:47One must observe with the utmost gravity that the current paradigm of therapeutic equivalence is fundamentally inadequate for the complexities of modern pharmacotherapy. The FDA’s Orange Book, while a commendable artifact of bureaucratic pragmatism, operates under the antiquated assumption that bioequivalence equates to clinical equivalence - a fallacy of the first order.
One cannot reduce the pharmacokinetic interplay of dual-active-agent formulations to a 90-111% confidence interval. Such reductionism is not merely insufficient - it is ethically negligent. The very notion that croscarmellose sodium and sodium starch glycolate are interchangeable excipients is a testament to the institutional decay of pharmaceutical oversight.
One must demand, with the gravitas befitting a medical professional, the establishment of a tiered equivalence classification system - one that accounts for excipient variance, dissolution profiles, and patient-specific metabolic phenotypes. Until then, we are not practicing medicine. We are playing Russian roulette with pill bottles.
Nina Stacey
December 23, 2025 AT 04:42OMG I just realized my grandma switched to a different generic of her blood pressure combo last month and she’s been super dizzy lately I thought it was just aging but now I’m scared
like why does the pill look different every time she gets it filled and no one ever tells you this stuff like why is this not on the label or something
also i work at a coffee shop and my coworker said her mom had a seizure after switching generics and no one believed her until she showed the ER the receipt
we need to talk about this more like why is this not common knowledge
also i think the FDA should make a chart with pictures of the pills and what fillers they use like a little icon system so you know if its safe or not
pls someone make this happen
Dominic Suyo
December 24, 2025 AT 12:16Let’s be real - the FDA’s ‘A’ rating is a corporate loophole dressed up as science. You think they care about your grandma’s dizziness? Nah. They care about how many generic pills they can push through the system before the next quarterly earnings call.
That ‘95% A-rated’ stat? It’s a mirage. It’s like saying 95% of cars have four wheels - doesn’t mean they won’t explode on a curve. And those NTI drugs? They’re the canaries in the coal mine, and we’re all pretending the smoke isn’t thick enough to choke on.
And don’t even get me started on the pharmacists who just scan and hand it over without blinking. They’re not professionals. They’re vending machines with stethoscopes.
Kevin Motta Top
December 25, 2025 AT 12:11Biggest thing I learned working in rural clinics: patients don’t care about TE codes. They care about whether they feel okay. If they feel weird after a refill, they don’t say ‘the disintegrant changed.’ They say ‘I think this medicine is broken.’
We need to train providers to ask that question - not ‘did you take it?’ but ‘did it feel the same?’
Simple. Human. Works.
William Liu
December 25, 2025 AT 15:18Just had a patient on levothyroxine/amlodipine combo switch generics last month. TSH jumped from 2.1 to 6.8. No symptoms at first. Then fatigue, weight gain, depression. Took three weeks to catch it. We switched back. Back to normal in two weeks.
This isn’t theoretical. It’s happening every day. And most doctors don’t even check labs after a switch.
Stop assuming. Start verifying.
Aadil Munshi
December 26, 2025 AT 01:20Ah yes, the great generic conspiracy. Let me ask you this - if two pills have the same active ingredients, why do we even need to overthink this? Is it because we’ve lost faith in science or just in ourselves?
Every culture has its superstitions. In America, it’s the fear of the generic pill. In India, we know that the body adapts. The liver doesn’t care if it’s made in New Jersey or Hyderabad - it only cares about the molecule.
But then again, maybe you’re right. Maybe we need 17 layers of bureaucracy to feel safe. Maybe we need a PhD to understand why your blood pressure changed after a refill.
Either way, I’ll take my $12 generic over your $120 brand any day. And my TSH is fine.