Rebound Congestion Risk Calculator
How Long Have You Used Nasal Decongestant Sprays?
Enter the number of consecutive days you've used nasal decongestant sprays (e.g., Afrin, Neo-Synephrine).
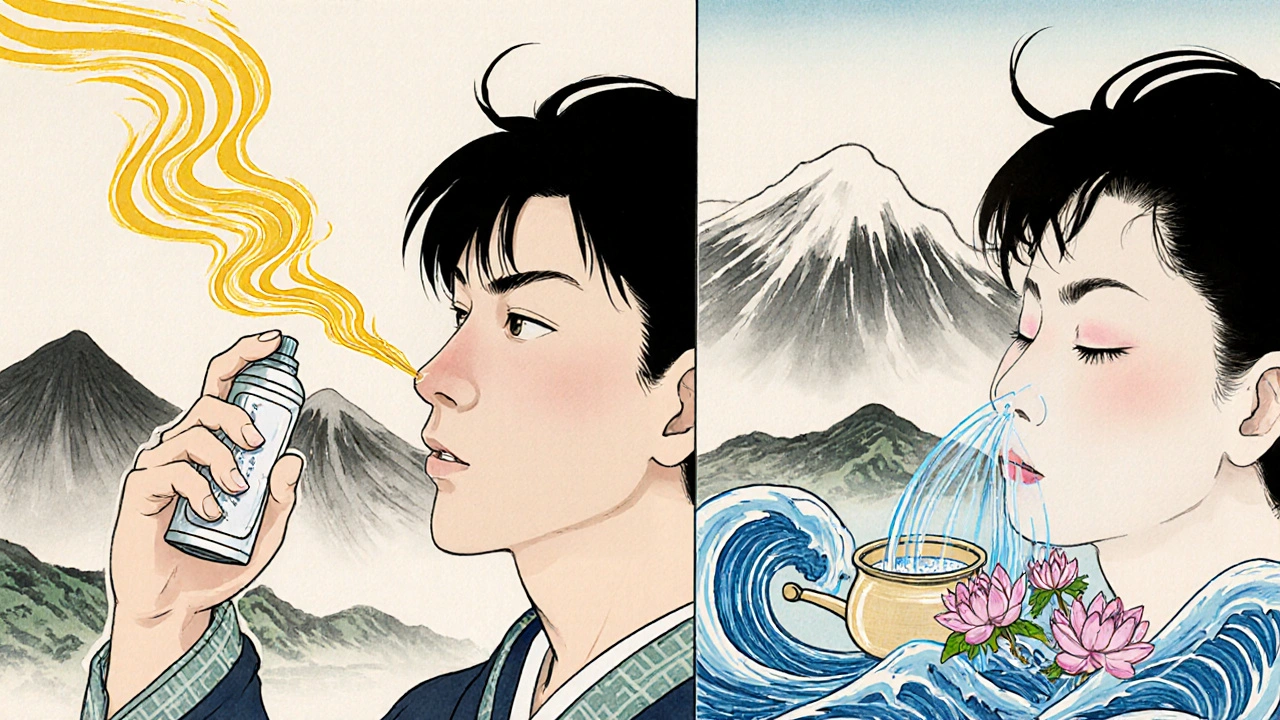
Ever used a nasal spray for a stuffy nose, only to find your congestion got worse after a few days? You’re not alone. This isn’t just bad luck - it’s a real medical condition called rhinitis medicamentosa, or rebound congestion. It happens when you use over-the-counter nasal decongestant sprays - like Afrin, Neo-Synephrine, or Xylometazoline - for more than three or four days. The spray works at first, shrinking swollen blood vessels in your nose. But when it wears off, those vessels swell back even bigger. Soon, you’re spraying more often just to breathe. And the cycle keeps getting worse.
How It Starts - And Why It Gets Worse
Most people don’t realize nasal decongestant sprays are meant for short-term use. The label says “use for up to 3 days,” but many people keep going because they feel better temporarily. The problem? Your nasal lining gets used to the medicine. It stops responding the same way. What was once relief becomes dependence. By day five or six, your nose feels more blocked than before you started. Studies show that over 90% of people who use these sprays beyond 10 days develop rebound congestion. The nasal tissue becomes inflamed, swollen, and sometimes even looks red or grainy when a doctor looks inside. In advanced cases, the lining can dry out, crack, and form crusts. You might start breathing through your mouth, wake up with a dry throat, or snore louder. Some people even develop nasal polyps - small, noncancerous growths - after months of overuse. The root cause is simple: vasoconstriction followed by rebound vasodilation. The spray shrinks blood vessels (vasoconstriction), but once it wears off, your body overcompensates by widening them even more (vasodilation). It’s like pulling a rubber band too far - it snaps back harder.The Only Way to Break the Cycle: Stop the Spray
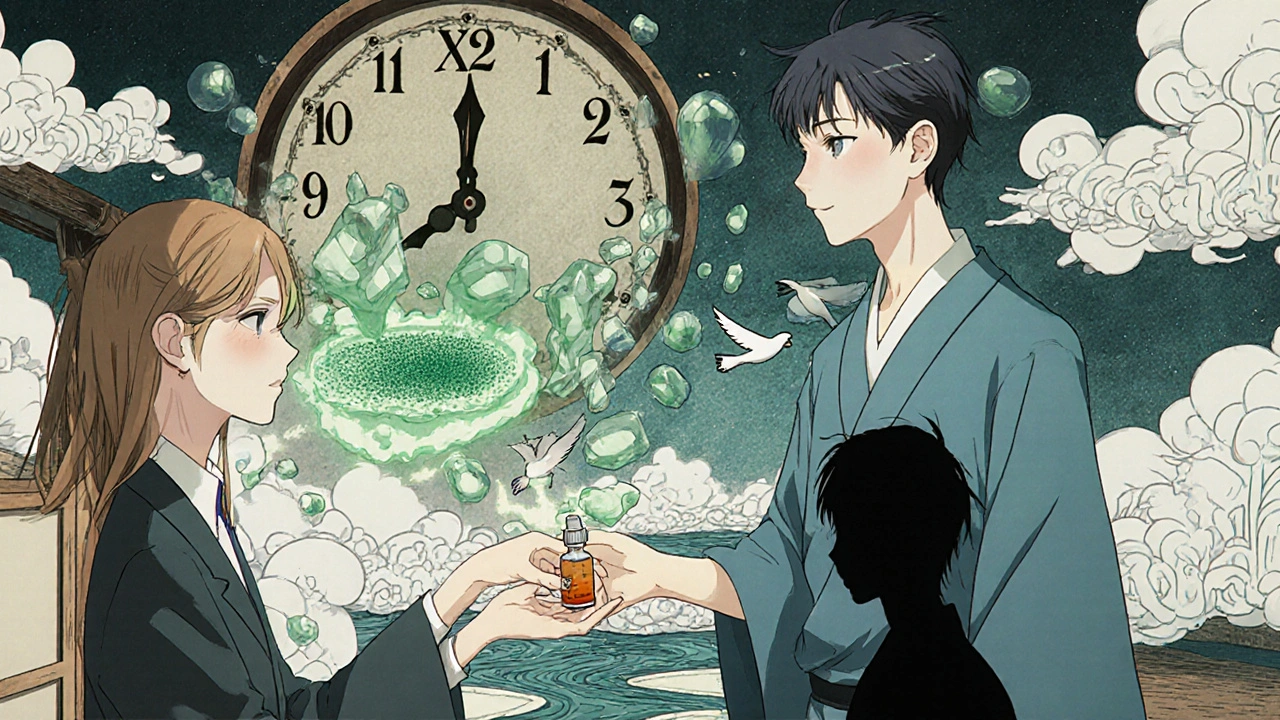
There’s no magic pill to fix this. The single most important step is to stop using the decongestant spray entirely. Sounds easy, right? It’s not. Withdrawal can be brutal. For the first 3-7 days, your congestion will likely get worse - sometimes dramatically. You might feel like you can’t breathe at all. Sleep becomes a challenge. But this is temporary. Your nose will heal - if you stick with it. Doctors have different approaches to stopping. The Mayo Clinic recommends quitting one nostril at a time. Spray only your left nostril for a few days, then stop. Once that side clears up, stop on the right. This helps you breathe through one side while the other heals. Many patients find this method much easier than stopping both at once. Cleveland Clinic, on the other hand, suggests gradually reducing use - cutting back from twice daily to once daily, then every other day - to ease the shock. But most experts agree: stopping completely works best in the long run. The key is patience. Your nose doesn’t heal overnight.What to Use Instead - Evidence-Based Relief
While you’re weaning off the decongestant, you need something to manage the symptoms. Here’s what actually works, backed by research:- Intranasal corticosteroids - These are the gold standard. Flonase (fluticasone) and Nasonex (mometasone) reduce inflammation in the nasal lining. Studies show 68-75% of patients see major improvement within 2-4 weeks of daily use. They don’t cause rebound congestion. Use them consistently - twice a day at first, then once daily as symptoms improve.
- Saline nasal irrigation - A simple saltwater rinse (using a neti pot or squeeze bottle) flushes out irritants and soothes swollen tissue. A 2022 review found it helped 60% of patients during withdrawal. Do it 2-3 times a day, especially in the morning and before bed.
- Short-term oral steroids - For severe cases, a 5-day course of prednisone (0.5 mg per kg of body weight) can cut inflammation fast. One 2021 trial showed 82% of patients had significant relief. This is usually reserved for people with extreme symptoms or those who haven’t responded to other treatments.
- Capsaicin spray - Found in some European treatments, capsaicin (the compound in chili peppers) desensitizes nerve endings in the nose. European trials show about 55% effectiveness. It’s not widely available in the U.S., but it’s being studied.
Don’t rely on oral decongestants like pseudoephedrine (Sudafed) as a substitute. They can raise blood pressure and cause jitteriness, especially in people with heart conditions. One study found 1 in 7 hypertensive patients had dangerous spikes in blood pressure after using them.
What Real People Say - Stories from Recovery
Patient experiences tell a clear story. On Reddit’s r/allergies, one user wrote: “After 3 weeks of Flonase and no Afrin, my nose finally cleared up - the first week was hell but worth it.” That’s typical. Most people who stick with the plan see big improvement within 14 days. But not everyone succeeds. About 18% of patients go back to the spray during withdrawal. Why? Lack of support. Cleveland Clinic found that patients who got clear instructions and follow-up counseling had a 7% relapse rate. Those who didn’t? 22% went back to the spray. The most common complaints during withdrawal: constant stuffiness, trouble sleeping, dry mouth, and fatigue. These aren’t signs you’re failing - they’re signs your body is healing.How to Prevent It From Happening Again
The best treatment is prevention. Here’s how to avoid rhinitis medicamentosa before it starts:- Never use nasal decongestant sprays for more than 3 days. This isn’t a suggestion - it’s a medical fact. The FDA now requires this warning to be printed in 10-point font on all OTC packaging.
- Use saline irrigation first. The American College of Allergy recommends rinsing your nose with salt water before reaching for any spray. It’s safe, cheap, and reduces the chance of rebound congestion by 40%.
- Know your triggers. Allergies, dry air, pollution, or sinus infections can cause congestion. If your stuffiness lasts longer than a week, see a doctor. You might need antihistamines, allergy shots, or antibiotics - not a decongestant spray.
- Ask your pharmacist. A 2022 study found only 28% of people got proper instructions when buying nasal sprays. Don’t assume you know how to use it. Ask: “Is this safe for more than 3 days?”
When to See a Doctor
You don’t need to suffer alone. See a healthcare provider if:- Your congestion lasts more than 10 days without improvement
- You’ve been using nasal spray for more than a week
- You have pain, fever, or thick yellow/green mucus (signs of infection)
- You’re having trouble sleeping or breathing through your nose
- You’ve tried stopping the spray but can’t manage the withdrawal
A doctor can confirm if you have rhinitis medicamentosa, rule out other causes like polyps or deviated septum, and give you a personalized plan. They can also prescribe stronger corticosteroids or refer you to an ENT specialist if needed.
The good news? Most people recover fully. Once you stop the spray and give your nose time to heal, it regains its normal function. The inflammation fades. The swelling goes down. Breathing returns. But you have to break the cycle - no shortcuts.
Can I use saline spray every day?
Yes. Saline nasal sprays or rinses are safe for daily, long-term use. They don’t cause rebound congestion and help keep your nasal passages moist and clean. Use them as often as needed - even multiple times a day - especially during cold and allergy season.
How long does rebound congestion last after stopping the spray?
Withdrawal symptoms usually peak between days 3 and 7 and start improving after day 7. Most people notice major relief within 10-14 days. Full recovery can take up to 4-6 weeks, especially if you’ve been using the spray for months or years. Patience and consistent use of corticosteroids or saline make a big difference.
Are there any natural remedies that help?
Humidifiers, staying hydrated, and steam inhalation (like from a hot shower) can ease dryness and discomfort. But they don’t treat the inflammation causing the congestion. For real relief during withdrawal, stick with saline irrigation and intranasal corticosteroids - they’re the only treatments proven to reduce swelling and speed healing.
Can children get rebound congestion from nasal sprays?
Yes. Children are just as vulnerable as adults, especially if parents use decongestant sprays without checking the label. Most OTC nasal sprays are not approved for kids under 6. Always check the age restrictions and talk to a pediatrician before using any nasal spray on a child.
Is it safe to use nasal spray once a week to prevent congestion?
No. Even occasional use can trigger rebound congestion over time. Your nasal lining doesn’t need a “maintenance” dose of decongestant. If you’re using it weekly, you’re likely masking an underlying issue like allergies or chronic sinusitis. See a doctor to find the real cause instead of relying on temporary fixes.
Next Steps: What to Do Today
If you’ve been using a nasal decongestant spray for more than a few days:- Stop using it - don’t wait for symptoms to get worse.
- Start saline rinses twice a day - use distilled or boiled water.
- Buy Flonase or Nasonex over the counter - use it as directed for at least 2 weeks.
- Track your progress - write down how your breathing feels each day.
- See a doctor if you’re not better in 10 days - you might need a stronger plan.
This isn’t a quick fix. But it’s a fix you can trust. Your nose can heal. You just have to give it the chance.

Johnson Abraham
November 14, 2025 AT 05:24Shante Ajadeen
November 15, 2025 AT 18:34dace yates
November 16, 2025 AT 09:14Renee Ruth
November 17, 2025 AT 23:22Samantha Wade
November 19, 2025 AT 13:36Elizabeth Buján
November 19, 2025 AT 13:52Andrew Forthmuller
November 21, 2025 AT 03:07vanessa k
November 21, 2025 AT 09:06manish kumar
November 21, 2025 AT 21:26Nicole M
November 22, 2025 AT 06:22Arpita Shukla
November 23, 2025 AT 08:34