Decongestant Safety Checker
Check Your Decongestant Safety
Enter the active ingredient you're considering to see if it's safe with your blood pressure medications.
Key Information
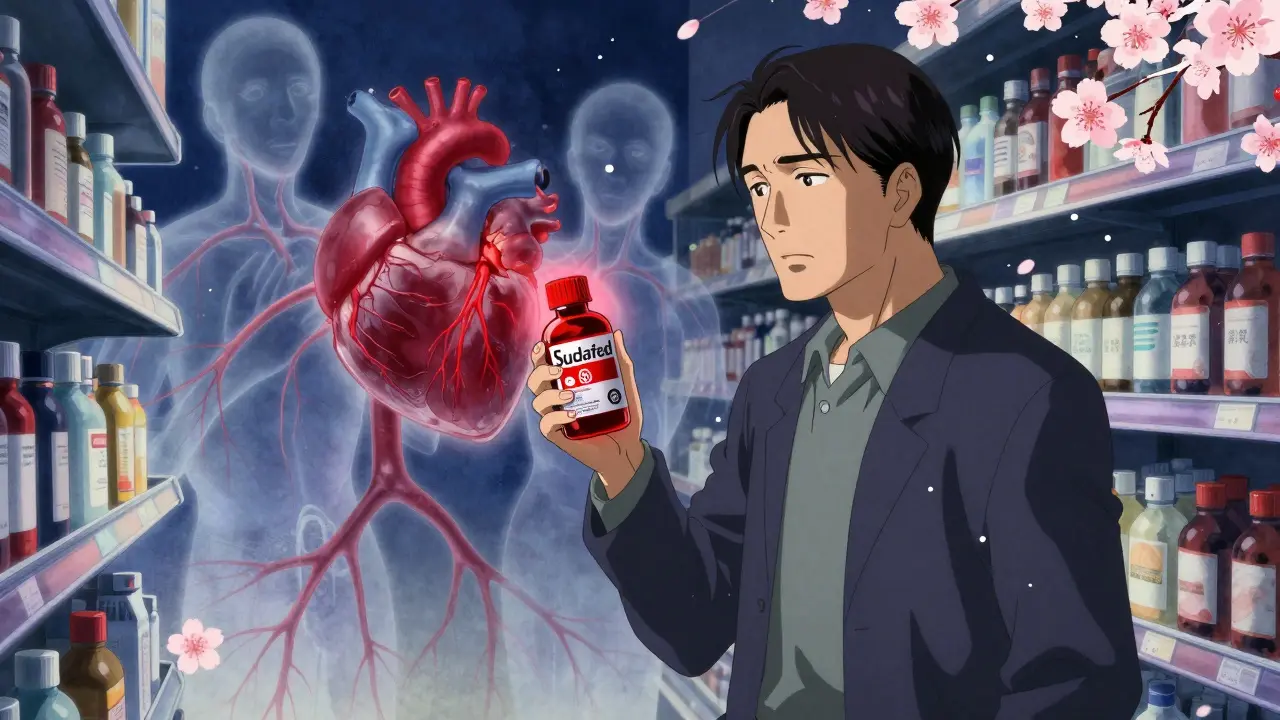
If you’re on blood pressure medication and you’ve got a stuffy nose, you might be tempted to grab the first decongestant off the shelf. But here’s the truth: that little bottle could be hiding a serious risk. Many common cold and flu remedies contain ingredients that can spike your blood pressure - even if you’ve been managing it well. This isn’t just a warning on a label. It’s a real, documented danger that sends people to the ER every year.
Why Decongestants Are Risky With High Blood Pressure
Nasal decongestants like pseudoephedrine and phenylephrine work by tightening blood vessels. That’s why your nose clears up - less swelling, less mucus. But that same effect doesn’t stay in your nose. These drugs circulate through your whole body, squeezing blood vessels everywhere, including those around your heart and brain. For someone with high blood pressure, this can mean a sudden, dangerous jump in blood pressure readings. The American Heart Association says this isn’t a small concern. Over 75 million adults in the U.S. have hypertension. And studies show that even a single dose of pseudoephedrine can raise systolic blood pressure by 2 to 5 mmHg on average - more in some people, especially with higher doses or immediate-release forms. In rare but documented cases, people with controlled hypertension have seen their blood pressure shoot up to dangerous levels after taking just one tablet. These drugs don’t just raise blood pressure. They can also make your heart race, cause palpitations, or even trigger abnormal heart rhythms. If you’re already on medications like beta-blockers (metoprolol), calcium channel blockers (felodipine, nifedipine), or ACE inhibitors, the interaction can be unpredictable. Sometimes the decongestant makes your blood pressure meds less effective. Other times, it causes a dangerous buildup of chemicals like norepinephrine, leading to spikes that even your doctor might not see coming.Which Decongestants Are the Biggest Concern?
Not all decongestants are created equal, but most over-the-counter ones carry the same red flags:- Pseudoephedrine - Found in Sudafed and many multi-symptom cold pills. This is the most potent and most studied. It’s behind the pharmacy counter in the U.S. for a reason.
- Phenylephrine - Now the most common decongestant in OTC products after pseudoephedrine was restricted. But studies show it’s just as risky for blood pressure, even if it’s less effective at relieving congestion.
- Oxymetazoline - Found in nasal sprays like Afrin. Many people think topical means safe. It doesn’t. A small amount gets absorbed into your bloodstream, and repeated use can still raise blood pressure.
- Ephedrine - Rare in the U.S. now, but still found in some supplements. Extremely dangerous with hypertension.
What Happens When You Mix Them?
A 2024 study in the Journal of Clinical Hypertension found that 22% of emergency visits for uncontrolled high blood pressure in adults over 50 were linked to OTC decongestant use. That’s not a coincidence. It’s a pattern. Take the case of a 62-year-old man on lisinopril for hypertension. He took a cold tablet with phenylephrine for three days because he “just wanted to sleep.” His blood pressure went from 128/82 to 185/105. He ended up in the ER with a pounding headache and blurred vision. His doctor said the decongestant had blocked the effect of his blood pressure medicine and pushed his arteries into overdrive. Even people who think their blood pressure is “under control” aren’t safe. The Cleveland Clinic says bluntly: “Don’t take nasal decongestants if you have unmanaged high blood pressure.” But they also warn: “They can raise your blood pressure even if you do have it managed.” And it’s not just decongestants. Many cold medicines are loaded with sodium - sometimes over 200 mg per tablet. The American Heart Association says high sodium intake can worsen hypertension. So you’re getting a double hit: vasoconstriction from the drug, and fluid retention from the salt.
Safe Alternatives for Congestion Relief
You don’t have to suffer. There are safer ways to clear your nose without risking your heart.- Nasal saline spray - Plain saltwater spray or neti pots. No drugs. No side effects. Just flushes out mucus and irritants. Use it several times a day.
- Steam and humidity - Take a hot shower. Use a humidifier. The warm, moist air loosens congestion naturally.
- Antihistamines - If your congestion is from allergies or post-nasal drip, drugs like loratadine (Claritin) or cetirizine (Zyrtec) can help. They don’t raise blood pressure. They work slower than decongestants, but they’re much safer.
- Hydration and rest - Drink water. Sleep. Let your body heal. Most colds resolve on their own in 7-10 days.
What to Do Before You Take Anything
If you’re on blood pressure medication, follow these steps before reaching for any OTC product:- Check every label - Look for pseudoephedrine, phenylephrine, oxymetazoline, or ephedrine. If you see any, skip it.
- Ask your pharmacist - They’re trained to spot dangerous interactions. Even if you buy pseudoephedrine behind the counter, they’re required to ask if you have high blood pressure. Use that moment. Say: “I’m on blood pressure meds. Is this safe?”
- Keep a medication list - Write down every prescription, supplement, and OTC drug you take. Bring it to every doctor’s visit.
- Monitor your blood pressure - If you absolutely must use a decongestant (only with your doctor’s OK), check your BP twice a day during use. Stop immediately if it rises more than 15 points above your usual.
- Don’t use nasal sprays longer than 3 days - Even saline is fine for longer. Oxymetazoline sprays can cause rebound congestion and worsen your symptoms if used too long.
When to Call Your Doctor
Don’t wait for a crisis. Call your provider if:- You’ve already taken a decongestant and feel dizzy, chest tight, or your heart is racing
- Your blood pressure reading is consistently above 140/90
- You’re unsure whether a cold medicine is safe
- You’ve had unexplained spikes in blood pressure recently

The Bigger Picture
Here’s the hard truth: about 30% of people with high blood pressure are unknowingly taking something that makes their condition worse. OTC meds are the #1 culprit. The American College of Cardiology is updating its 2026 guidelines to include stronger warnings about over-the-counter drugs - because this problem is growing. Pharmacists who do medication reviews have cut inappropriate decongestant use by 47% in studies. That means education works. But it only works if you ask. Don’t assume your doctor knows what you’re taking. Don’t assume the pharmacist will stop you unless you speak up. And don’t think “it’s just one pill.” One pill can be enough.Frequently Asked Questions
Can I use a saline nasal spray if I have high blood pressure?
Yes, saline nasal sprays are completely safe for people with high blood pressure. They contain no medication - just salt and water. They help flush out mucus and reduce swelling without affecting your blood pressure or interacting with your medications. Use them as often as needed.
Is phenylephrine safer than pseudoephedrine?
No, phenylephrine is not safer. While it’s less effective at relieving congestion, it still raises blood pressure in people with hypertension. The FDA and American Heart Association treat both drugs as equally risky for those on blood pressure medication. Avoid both unless your doctor specifically approves one.
Can I take decongestants if my blood pressure is under control?
Even if your blood pressure is controlled, decongestants can still cause dangerous spikes. The Cleveland Clinic and Mayo Clinic advise against using them at all if you have hypertension. If you absolutely must use one, do so only under your doctor’s supervision, at the lowest dose, for no more than 2-3 days.
Do antihistamines raise blood pressure?
Most second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) do not raise blood pressure. They’re a safer option for congestion caused by allergies. Avoid first-generation antihistamines like diphenhydramine (Benadryl) - they can cause drowsiness and may interact with other meds.
What should I do if I accidentally took a decongestant?
Stop taking it immediately. Check your blood pressure. If it’s more than 20 points above your normal reading, or if you feel chest pain, dizziness, or a rapid heartbeat, seek medical help right away. Even if you feel fine, call your doctor or pharmacist to discuss what to do next. Don’t wait for symptoms to get worse.
Next Steps
If you’re on blood pressure medication:- Review your medicine cabinet today. Toss anything with pseudoephedrine, phenylephrine, or oxymetazoline.
- Keep a bottle of saline spray and a humidifier on hand for cold season.
- Ask your pharmacist to review all your OTC meds during your next visit.
- Set a reminder to check your blood pressure weekly - especially during cold and flu season.
Jeane Hendrix
January 5, 2026 AT 21:20Okay but like... why is phenylephrine even still in anything? I read that study where it’s basically a placebo for congestion but still spikes BP like it’s trying to win a competition. My grandma took it last winter and ended up in the ER. She didn’t even know what was in the NyQuil. We all assume ‘OTC’ means ‘safe’ but nope. 😔
Gabrielle Panchev
January 6, 2026 AT 18:33Look, I get it-decongestants are bad, but let’s be real: the real problem here isn’t the drugs, it’s the fact that people don’t read labels, don’t talk to pharmacists, and think ‘if it’s on the shelf, it’s fine.’ I’ve seen people buy Sudafed behind the counter, lie about their BP, and then wonder why they’re dizzy. It’s not the medication’s fault-it’s the human behavior. Also, saline sprays? Sure, they work-but they’re boring. Nobody wants to spray salt water when they can just pop a pill. And that’s the cultural problem right there.
Venkataramanan Viswanathan
January 8, 2026 AT 13:20In India, we rarely use pseudoephedrine. Most people rely on steam inhalation, turmeric milk, or nasal irrigation with warm salt water. Even in urban pharmacies, decongestants are not the first recommendation. We understand that hypertension is serious. But I notice in the U.S., convenience often overrides caution. This article is important. But awareness must come from community education-not just medical warnings.
Kiran Plaha
January 8, 2026 AT 15:42I didn’t know phenylephrine was just as bad as pseudoephedrine. I thought the new stuff was safer. Thanks for clarifying. I’ve been using those DayQuil bottles for years. Going to toss them tonight. Saline spray is my new best friend now. Simple, cheap, no drama. Good post.
Matt Beck
January 9, 2026 AT 15:49It’s not just about BP… it’s about the illusion of control. We think we’re managing our health by popping pills, but we’re just outsourcing our biology to Big Pharma’s marketing department. 🤖💊 The real cure? Accepting that being sick is part of being human. Let your body breathe. Let your nose run. Let your soul rest. You don’t need to ‘fix’ everything with chemicals. Sometimes… just breathe.
Kelly Beck
January 10, 2026 AT 18:41Y’all, I’m so proud of this post!! 💪 Seriously, this is the kind of info we NEED more of. I showed this to my mom and she’s now using a humidifier and saline spray instead of her old cold meds. And guess what? She slept better, didn’t get dizzy, and didn’t spike her BP. Small changes, huge impact. You’re not alone if you’ve been using decongestants for years-just start today. One less pill, one more breath. You got this! 🌿💧
Katie Schoen
January 11, 2026 AT 00:49So let me get this straight: the FDA made pseudoephedrine behind-the-counter because people were making meth… but phenylephrine? Oh, that’s totally fine. Just keep selling it like it’s a miracle cure. Classic. 😒 Meanwhile, my sinuses are still clogged and my BP is still high. Thanks, America.
Tiffany Adjei - Opong
January 12, 2026 AT 10:44Okay, but have you considered that maybe the real issue is that people with hypertension shouldn’t be getting colds in the first place? Like, if you’re managing your BP properly, your immune system should be stronger. Maybe the problem isn’t the decongestants-it’s that you’re not eating right, sleeping enough, or reducing stress? Just saying. Also, saline spray? That’s like… 1990s medicine. Have you tried a neti pot with essential oils? That’s real relief.
Ryan Barr
January 12, 2026 AT 23:16Decongestants = bad. Saline = good. Done.
Cam Jane
January 14, 2026 AT 14:21Just wanted to add-this isn’t just about cold season. I’m a nurse, and I see this every spring and fall. People with asthma + hypertension use OTC decongestants for allergy congestion and then end up in the ER with tachycardia. The saline spray + humidifier combo works better than 90% of meds anyway. And if you’re using nasal sprays longer than 3 days? You’ve got rebound congestion. It’s not your nose-it’s the spray. Stop. Reset. Breathe. I’ve had patients cry because they didn’t know this. You’re not alone. And you’re not weak for needing help. Just be smart. 🩺❤️