Most people think pain means something is broken. If your back hurts, you assume there’s damage. If your knee aches, you believe the joint is worn out. But what if that pain isn’t a warning signal from damaged tissue - but a false alarm from your brain?
Why Your Brain Makes Pain Even When You’re Not Hurt
Pain isn’t just a message from your body to your brain. It’s a full-blown output your brain creates based on what it thinks is dangerous. This is the core idea behind pain neuroscience education (PNE). It’s not about fixing your spine, kneecap, or muscle. It’s about changing how your brain interprets signals - even when those signals are turned up too high. For decades, pain was treated like a broken pipe. If you had chronic pain, doctors looked for structural problems: herniated discs, arthritis, torn ligaments. But here’s the problem: many people with severe pain have no visible damage. And many people with major damage on an MRI feel no pain at all. That’s not a mistake. That’s biology. The brain doesn’t measure damage. It measures threat. If your nervous system has been on high alert for months or years - because of injury, stress, fear, or even past trauma - it starts to overreact. Tiny movements, normal stiffness, or even just thinking about movement can trigger a pain response. This is called central sensitization. Your nervous system becomes hypersensitive, like a smoke alarm that goes off every time you burn toast.How Pain Neuroscience Education Works
Pain neuroscience education doesn’t tell you to ignore your pain. It tells you to understand it. The goal is to help you see pain not as a sign of damage, but as a sign of your nervous system being overly protective. The most common way this is done is through simple metaphors. One popular one compares your nervous system to a smoke alarm. A healthy alarm only goes off when there’s real fire. But a sensitive alarm goes off with burnt toast, steam from the shower, or even dust. That doesn’t mean the alarm is broken - it just needs recalibration. Another metaphor is the “pain thermostat.” Think of your nervous system like a house with a thermostat set too high. Even when the room is comfortable, the heater keeps running because the thermostat thinks it’s freezing. PNE helps you lower that thermostat - not by fixing the heater, but by teaching your brain the room is safe. These ideas are backed by real science. Brain scans show that after PNE, areas linked to threat detection - like the amygdala and insula - become less active. At the same time, areas responsible for rational thinking - like the prefrontal cortex - become more engaged. In short: your brain starts to trust your body again.What the Research Says
Over 20 systematic reviews and meta-analyses have looked at PNE. The results are consistent: people who learn about pain neuroscience report less pain, less fear of movement, and better function - even if their MRI still shows “degenerative changes.” One 2023 review of 23 clinical trials found that PNE reduced pain intensity by an average of 1.8 points on a 10-point scale. That might not sound like much, but in chronic pain, even a 1-point drop is considered meaningful. More importantly, disability improved by over 12%, and pain catastrophizing - the tendency to magnify pain and feel helpless - dropped by 6.2 points on a standard scale. But here’s the key: PNE works best when it’s not alone. When combined with movement therapy - like graded exercise or physical activity - outcomes improve by 30-40%. That’s because once your brain stops seeing movement as dangerous, you can start moving again. And movement is one of the most powerful pain modulators we have.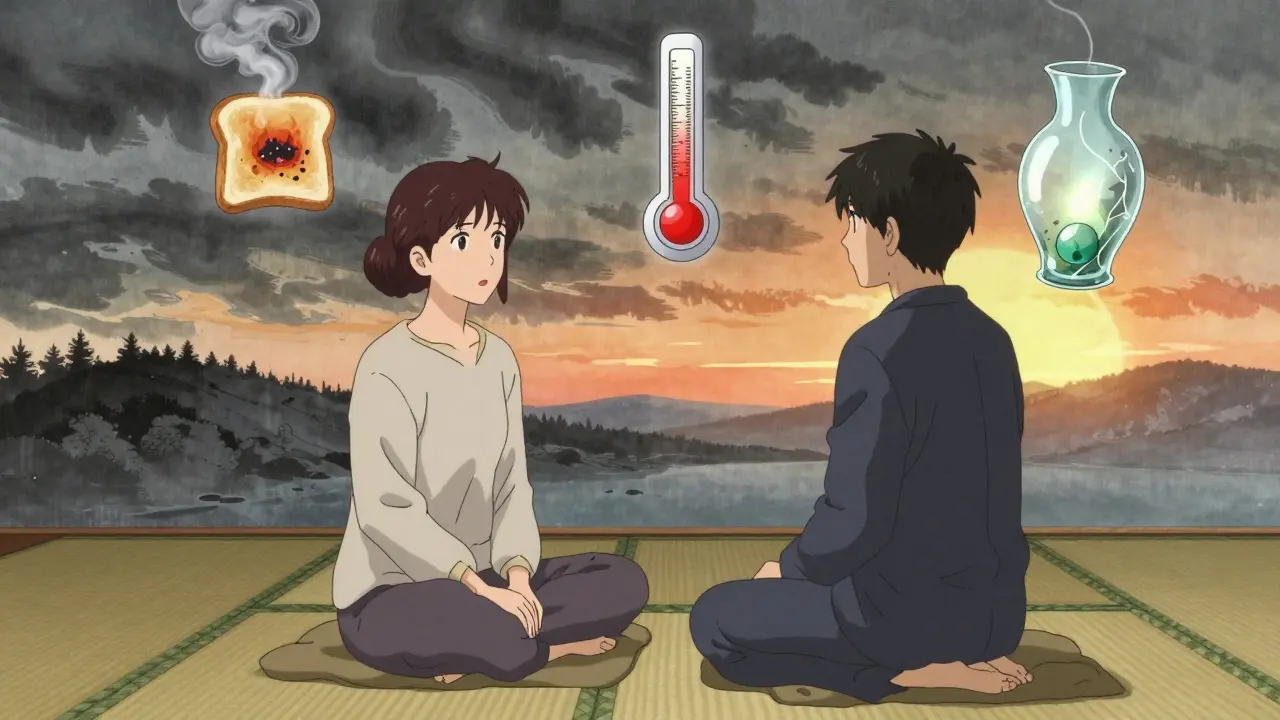
Who Benefits Most - and Who Doesn’t
PNE isn’t a magic fix for everyone. It’s most effective for chronic pain conditions - especially low back pain, fibromyalgia, complex regional pain syndrome, and persistent neck or shoulder pain. In these cases, tissue damage is rarely the main driver. The nervous system is. But for acute pain - like a broken bone or recent surgery - PNE has limited value. If your body is truly injured, you need healing, not retraining. Studies show PNE helps in only 11% of acute cases, compared to 82% for chronic pain. It also doesn’t work well for people with severe cognitive impairment or very low health literacy. If someone can’t grasp the idea that pain isn’t always damage, the metaphors fall flat. In those cases, simpler language - like “your body’s alarm system is too sensitive” - works better than terms like “neuroplasticity” or “central sensitization.” And some people just don’t buy it. If you’re expecting PNE to make your pain disappear overnight, you’ll walk away disappointed. This isn’t a quick fix. It’s a mindset shift. One patient on Reddit said: “After six months of fearing every movement would tear me apart, the smoke alarm metaphor finally clicked. I started walking again. I cut my pain meds by 75%.” That didn’t happen in one session. It happened because he kept showing up, kept learning, and kept moving.How It’s Done in Practice
PNE is usually delivered in 30-45 minute sessions by physical therapists, occupational therapists, or pain specialists trained in the approach. The most common models are “Explain Pain” by David Butler and Lorimer Moseley, and “Therapeutic Neuroscience Education” by Adriaan Louw. Both use stories, diagrams, and analogies - not textbooks. A typical session might include:- Explaining how nerves send signals, but the brain decides whether to make pain
- Showing how stress, sleep, and emotions affect pain
- Using diagrams of the nervous system - not to overwhelm, but to clarify
- Linking pain to behavior: “When you avoid movement because you fear damage, your body gets weaker, your brain gets more scared, and your pain gets louder”

Why Most Clinicians Still Don’t Use It
Despite strong evidence, only 28% of physical therapists in the U.S. say they feel confident delivering PNE. Why? First, it takes time. Most clinics are under pressure to see 10+ patients a day. Teaching someone about neurobiology doesn’t fit neatly into a 15-minute slot. Second, many clinicians were trained in the old model: “Find the injury, fix the injury.” Shifting to a brain-based model feels uncomfortable - even threatening. Some worry patients will think they’re being told their pain isn’t real. Third, there’s no single certification. While the International Spine and Pain Institute offers a 24-hour course, it’s not required. Many therapists learn on their own through books, workshops, or online courses. But change is coming. Since 2021, Medicare has started reimbursing PNE under physical therapy codes. Over 70% of U.S. physical therapy programs now teach it in school - up from just 12% in 2010. And 41 Fortune 100 companies now use PNE principles in their workplace injury programs, reporting a 22% drop in workers’ comp claim duration.What You Can Do Right Now
You don’t need a therapist to start learning. If you’ve had pain for more than three months and doctors haven’t found a clear structural cause, try this:- Read Explain Pain by David Butler and Lorimer Moseley. It’s written for patients, not doctors.
- Watch the free YouTube videos by Lorimer Moseley. He explains pain using simple animations and stories.
- Ask yourself: “Do I avoid movement because I’m afraid of damage - or because it actually hurts?”
- Start moving gently, even if it hurts a little. Pain doesn’t mean damage. Discomfort doesn’t mean danger.
- Track your pain not just in intensity, but in how much it limits your life.
What’s Next for Pain Neuroscience Education
Researchers are now testing PNE for acute pain after surgery, using virtual reality to deliver lessons, and even matching PNE content to individual brain patterns. One NIH-funded trial is exploring whether PNE can reduce opioid use after surgery by helping patients understand that pain doesn’t equal harm. The future of pain care isn’t more scans, more pills, or more injections. It’s better understanding. When your brain learns that your body isn’t under attack - that it’s safe to move, to breathe, to live - pain loses its power.Is pain neuroscience education only for back pain?
No. While it’s most commonly used for chronic low back pain, PNE has been shown to help with fibromyalgia, neck pain, shoulder pain, complex regional pain syndrome, and even persistent headaches. Any condition where pain continues long after tissue healing should be considered for PNE.
Can I do pain neuroscience education on my own?
Yes. Many people learn effectively through books like Explain Pain, free videos by Lorimer Moseley, or apps like Pain Revolution. But working with a trained clinician improves outcomes. They can tailor the message to your experience, answer questions, and connect the ideas to your movement habits.
Will PNE make my pain disappear?
Not always. But it often makes pain less scary and less limiting. Many people report they still feel pain sometimes, but they no longer fear it. They can walk, sleep, work, and enjoy life again - even with some discomfort. That’s the real win.
Is pain neuroscience education the same as CBT?
They’re different. Cognitive behavioral therapy (CBT) focuses on changing thoughts and behaviors around pain. PNE focuses on changing your understanding of pain itself - specifically, teaching you that pain is a protective output of the brain, not a direct measure of damage. Many people benefit from both.
Why do some people say PNE didn’t work for them?
The most common reason is unrealistic expectations. If you expect PNE to erase pain in one session, you’ll be disappointed. It’s not a treatment - it’s a learning process. Others find the science too complex. Good PNE uses simple language and relatable stories. If it felt like a lecture, it wasn’t delivered well.

Lana Kabulova
January 22, 2026 AT 12:52I’ve had chronic back pain for 8 years-MRI shows ‘degenerative changes’ everywhere… but I can deadlift 200lbs now. I used to think pain = damage. Now I know it’s just my nervous system screaming ‘DANGER!’ when I breathe too hard. The smoke alarm metaphor? Perfect. I finally stopped avoiding stairs. I’m not pain-free-but I’m life-full again.
Keith Helm
January 22, 2026 AT 16:47It is imperative to note that the efficacy of pain neuroscience education is contingent upon the patient’s cognitive capacity to assimilate abstract neurobiological constructs. Without adequate baseline literacy, the intervention is fundamentally flawed.
Alec Amiri
January 24, 2026 AT 03:36LMAO so now we’re telling people their pain is ‘all in their head’? 😂 Classic. Next they’ll say your broken leg is just your brain being dramatic. I’ve seen guys cry from a stubbed toe-your brain ain’t lying, it’s just doing its job. Stop gaslighting chronic pain patients. You want them to move? Then fix the damn tissue. Not their mindset.
Akriti Jain
January 25, 2026 AT 02:12Of course the pharmaceutical companies HATE this 😏 They make billions off pills and surgeries. But the real secret? The government’s been funding this since 2015… and they don’t want you to know. 🤫 Your pain? It’s a distraction. Wake up. 🌍💊 #PainIsABigLie
Patrick Roth
January 26, 2026 AT 02:29Everyone’s acting like this is some revolutionary breakthrough. I’ve been saying this since 2012. Pain is a perception. You think you’re the first person to realize the brain generates pain? Newsflash: Descartes knew. The Greeks knew. Even ancient Ayurveda knew. You just needed a fancy acronym and a TED Talk to get paid for it.
Oren Prettyman
January 27, 2026 AT 12:54While the theoretical framework presented herein is not without merit, the empirical evidence cited appears to be selectively aggregated from a narrow corpus of meta-analyses, predominantly from institutions with vested interest in non-pharmacological interventions. The statistical significance of a 1.8-point reduction on a 10-point scale, when contextualized against the heterogeneity of chronic pain populations, remains methodologically questionable. Furthermore, the implicit dismissal of structural pathology as irrelevant is not only scientifically premature but potentially hazardous in clinical practice.
Tatiana Bandurina
January 28, 2026 AT 08:26You know what’s worse than pain? Being told your pain isn’t real by someone who’s never felt it. I’ve had fibromyalgia for 15 years. I’ve been told I’m ‘too emotional,’ ‘just stressed,’ ‘not trying hard enough.’ This ‘education’ feels like another way to gaslight people into suffering silently. If your solution is ‘just move more,’ then you don’t understand what chronic pain actually is.
Philip House
January 29, 2026 AT 19:21Look, I get it. The brain’s a complex organ. But let’s not pretend this is some deep truth the medical establishment’s been hiding. It’s just another buzzword to sell books and courses. You think your amygdala’s scared? Mine’s been scared since 2008. I’ve been through three surgeries, two failed spinal fusions, and I still limp. You think a metaphor’s gonna fix that? Nah. What fixes it? Time. And maybe, just maybe, a little more respect for the body’s actual damage.
Hilary Miller
January 31, 2026 AT 02:58My mom in India had chronic knee pain for 10 years. Doctors said ‘wear a brace.’ Then she watched a Moseley video in Hindi. She started walking again. No surgery. No pills. Just… understanding. This isn’t just Western science-it’s human. And it works.
Margaret Khaemba
January 31, 2026 AT 21:59Just wanted to say thank you for this. I’ve been reading Explain Pain for 3 months now. It didn’t make my pain vanish-but it made me stop fighting it. I still feel it when I sit too long, but now I say ‘oh, that’s just my alarm system being extra.’ And I keep going. That’s the win. I’m not cured. But I’m not scared anymore. 💙