Ever picked up a prescription and stared at the little sticker on the bottle like it was a secret code? You’re not alone. Those small, often overlooked labels aren’t just paperwork-they’re lifelines. A single misunderstood warning can land you in the ER. In the U.S., medication errors cause over 1.3 million injuries every year. Most of them? Happen because someone didn’t understand what the sticker meant.
What Those Colored Stickers Are Really Saying
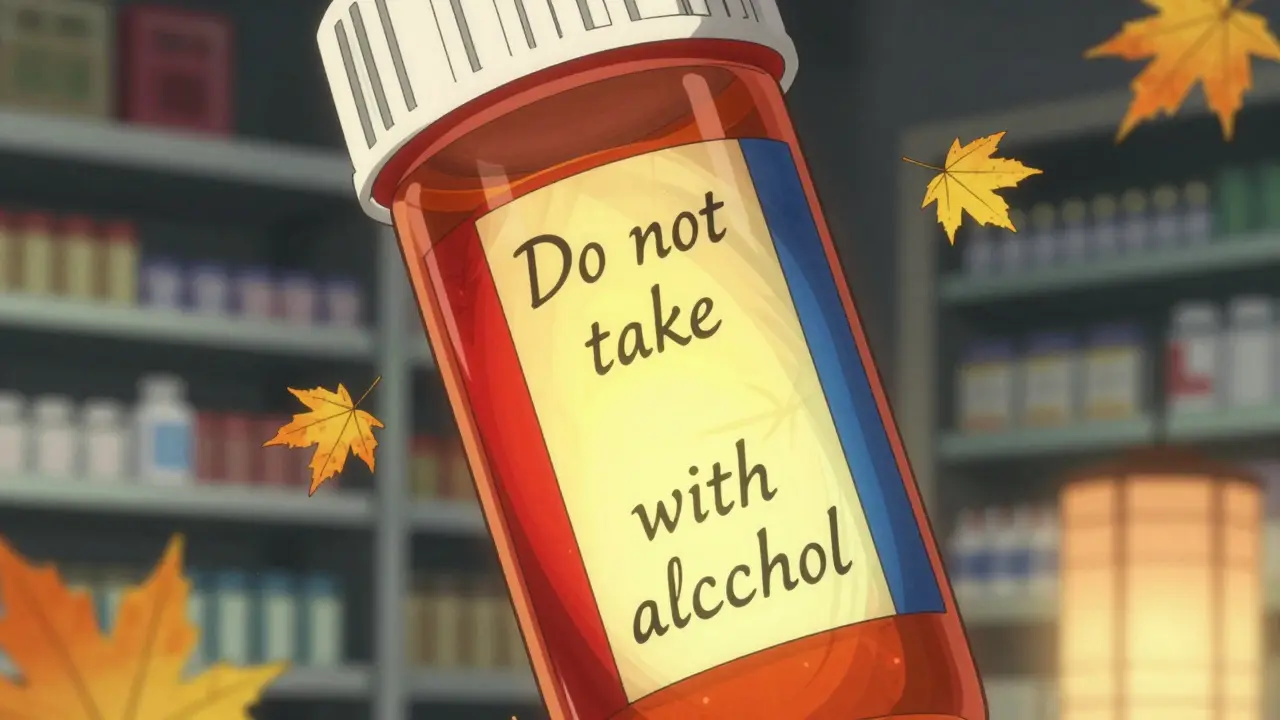
You’ve seen them: red, yellow, blue, white. They’re not random. Pharmacies use color to signal urgency. Red means danger. If you see a red sticker that says "Do not take with alcohol" or "May cause severe dizziness", this isn’t a suggestion. It’s a red flag. A 2017 study found that 85% of patients correctly understood red labels as serious risks. Yellow? That’s caution. Think "Take with food" or "May cause drowsiness". It’s not life-threatening, but ignoring it could make your medicine less effective-or worse, dangerous over time.Blue, white, and green? Those are usually reminders, not warnings. "Refrigerate" or "Take on empty stomach" fall here. People often skip these because they don’t feel urgent. But if you’re supposed to keep your antibiotic cold and leave it on the counter, it could lose its power. Same with taking a pill on an empty stomach-eating too soon can block absorption. These aren’t "nice to know" details. They’re part of how the drug works.
The Black Box Warning: When a Drug Can Kill
The most serious warning isn’t even on the sticker. It’s printed in bold black letters at the top of the prescribing info inside the box. It’s called a Boxed Warning. The FDA requires it when a drug has been linked to death or serious injury. About 40% of new drugs approved between 2013 and 2017 carried one. These aren’t rare. Common examples include blood thinners that can cause internal bleeding, diabetes drugs that increase heart failure risk, or antidepressants linked to suicidal thoughts in young adults.Here’s the catch: most patients never see this warning. It’s not on the bottle. It’s in the thick paper insert that gets tossed in the trash. That’s why pharmacists are trained to verbally explain it. If your doctor prescribes a drug with a Boxed Warning, ask: "What’s the biggest risk I need to watch for?" Don’t assume it’s covered by the sticker. The sticker might say "Take as directed"-but the real danger is hidden in the fine print.
Why "Swallow Whole" Means Exactly That
One of the most common-and most misunderstood-warnings is "Do not chew, crush, or break". On Reddit’s r/Pharmacy, pharmacists say nearly 30% of patients think this means "chew it up so it dissolves faster." That’s the opposite of what it means. These pills are designed to release medicine slowly. Crush them, and you get a full dose all at once. For opioid painkillers, that can cause an overdose. For extended-release blood pressure meds, it can crash your heart rate.Same goes for "Take on empty stomach". It doesn’t mean "don’t eat breakfast." It means wait at least one hour before eating or two hours after. Some antibiotics, like tetracycline, bind to calcium in milk or yogurt and become useless. Grapefruit juice? It can interfere with over 85 medications, including statins and blood pressure drugs. One patient in a Drugs.com forum said they threw away the paper warning about grapefruit juice-and ended up in the ER with dangerously low blood pressure.

Why Symbols Don’t Work (And What Does)
You’ve seen the icons: a glass with a line through it for "avoid alcohol," a car for "do not drive." The FDA tried using symbols to make labels universal. It backfired. A 2017 study found that 32% of people thought the "external use only" symbol meant "radioactive." Another 28% thought it meant "shaking or chills." Symbols alone only work for 65% of people.The best solution? Verbal explanation + simple text. A study showed that when a pharmacist says "This will make you sleepy, so don’t drive," while pointing to the yellow sticker, comprehension jumps to 92%. That’s why Kaiser Permanente’s pilot program-where pharmacists spend three extra minutes explaining each new prescription-saw patient understanding rise from 55% to 89%. The American Medical Association calls this the "teach-back" method: ask the patient to repeat the instruction in their own words. If they say, "So I can’t drink wine with this?" instead of "I can’t have alcohol", you know they got it.
Who’s Responsible When a Warning Gets Ignored?
It’s easy to blame the patient. But here’s the truth: the system is broken. Eighty million American adults have trouble reading health materials. That’s not laziness-it’s a lack of access to clear information. A 2021 study found that 68% of patients throw away the Patient Prescribing Information sheet because it’s too long, too technical, or printed in tiny font.Pharmacies are under pressure. The average patient spends just 7 to 12 seconds looking at their label. That’s less time than it takes to read this sentence. Independent pharmacies often lack training or time to explain. Chain pharmacies like Walgreens have "Medication Safety Check" programs that boost understanding to 92%. But most don’t. The FDA admits its current labeling system doesn’t work for people with low health literacy. And pharmaceutical companies? Internal documents show 73% opposed FDA efforts to simplify labels between 2018 and 2020-fearing lawsuits more than patient harm.

What You Can Do Right Now
You don’t need a medical degree to stay safe. Here’s what to do every time you pick up a prescription:- Check the color. Red = stop and ask. Yellow = be careful. White/blue = follow instructions.
- Match the pill. Is it the right shape, color, and imprint? If it looks different from last time, ask if it’s the same drug.
- Ask the pharmacist. Say: "What’s the one thing I absolutely must not do with this medicine?" That’s the most important warning.
- Use the teach-back method. After they explain, say: "So if I take this with grapefruit, I could get dizzy?" If they say yes, you got it.
- Keep the insert. Don’t toss it. Even if it’s long, scan for the "Warnings" and "Contraindications" sections. Highlight the red flags.
What’s Changing in 2025 and Beyond
The FDA is finally fixing this. Starting in 2025, 20 high-risk drug classes-including blood thinners, diabetes meds, and antidepressants-must come with a new "Facts Label." It’s a one-page, plain-language summary in big font, with icons and bullet points. It’s being tested now. Early results show patients understand it 50% better than the old inserts.Some pharmacies are testing QR codes on labels. Scan it, and a 60-second video explains the warning in simple terms. Mayo Clinic’s trial showed comprehension jumped 52%. By 2026, most experts expect these simplified labels to become standard.
But until then? You’re the last line of defense. Don’t assume. Don’t guess. Ask. Even if it feels awkward. A few extra seconds could save your life.
What does a red sticker on a prescription bottle mean?
A red sticker means there’s a serious risk that could lead to injury or death. These are urgent warnings like "Do not take with alcohol," "May cause severe dizziness," or "Risk of liver damage." Never ignore a red label. If you’re unsure, call your pharmacist immediately.
Why do some pills say "Do not crush or chew"?
These pills are designed to release medicine slowly over time. Crushing or chewing them releases the full dose all at once, which can be dangerous-or even deadly. For example, crushing an opioid painkiller can cause an overdose. Always swallow these pills whole, even if they’re hard to swallow.
Can I ignore a warning if I’ve taken the medicine before without problems?
No. Your body changes. Other medications you take may interact differently now. A warning like "Avoid grapefruit" might not have mattered last year, but if you started a new blood pressure drug this month, grapefruit could cause your blood pressure to drop dangerously low. Always treat every warning as new.
What’s the difference between "contraindicated" and "warning"?
"Contraindicated" means you must not take the drug at all under certain conditions-like if you have kidney failure or are pregnant. A "warning" means there’s a risk you need to manage, but you can still take the drug with care. For example, "Do not use if you have a history of heart attack" is a contraindication. "May cause drowsiness" is a warning.
Do I need to read the whole paper insert that comes with my medicine?
You don’t need to read every word, but you should scan the "Warnings and Precautions" and "Contraindications" sections. Look for anything that applies to you-your age, other meds, health conditions. If you see something confusing, ask your pharmacist to explain it. Don’t throw the insert away. Keep it for future reference.
Are there apps or tools to help me understand my prescription labels?
Yes. Apps like Medisafe, MyTherapy, and the FDA’s MedGuide app let you scan your pill or enter your prescription to get plain-language explanations of warnings and interactions. Some pharmacies also offer QR codes on labels that link to video explanations. If your pharmacy doesn’t offer this, ask if they can provide a printed summary in larger font.
What to Do If You Made a Mistake
If you took your medicine wrong-chewed a pill you shouldn’t have, drank alcohol with a warning, skipped a dose because you didn’t understand the label-don’t panic. Don’t hide it. Call your pharmacist or doctor right away. Most side effects are manageable if caught early. Pharmacists are trained to help you, not judge you. One call could prevent an emergency.Prescription labels are meant to protect you. But they only work if you understand them. Take the time to learn what each sticker means. Ask questions. Keep the insert. Use the teach-back method. Your health isn’t something you can afford to guess about.
Kuldipsinh Rathod
December 27, 2025 AT 01:55I used to ignore those red stickers until my uncle ended up in the hospital after mixing his blood pressure med with whiskey. Now I read every word. Seriously, if it says 'do not take with alcohol,' don't even think about it. Your body doesn't care how 'chill' you are.
SHAKTI BHARDWAJ
December 27, 2025 AT 10:56OMG THIS IS SO TRUE I JUST TOOK MY ANTIBIOTIC WITH MILK BECAUSE I WAS HUNGRY AND NOW I FEEL LIKE A ZOMBIE AND MY PHARMACIST LAUGHED AT ME AND I CRIED IN THE PARKING LOT AND NOW I HATE EVERYTHING
Matthew Ingersoll
December 27, 2025 AT 23:22The FDA's boxed warning system is a relic of a bygone era. Pharmaceutical companies have too much influence over labeling standards, and the current format assumes a level of health literacy that simply doesn't exist for millions of Americans. We need mandatory plain-language summaries, not more symbols that mean nothing to half the population.
carissa projo
December 29, 2025 AT 11:46There’s something deeply human about how we treat medication labels like cryptic scrolls from a forgotten temple. We stare at them, half-terrified, half-hoping they’ll magically explain themselves. But the truth? They’re not meant to be read alone. They’re meant to be held up to the light of a pharmacist’s voice, a nurse’s patience, a loved one’s quiet reminder. The real breakthrough isn’t in new fonts or QR codes-it’s in making space for someone to sit with you while you read it. That’s the teach-back method. That’s care.
josue robert figueroa salazar
December 30, 2025 AT 03:31People die because they don’t read. End of story. Stop blaming the system.
david jackson
December 30, 2025 AT 05:10Let me tell you about the time I crushed my extended-release oxycodone because I thought it’d work faster-turns out, it didn’t work faster, it worked TOO FAST. I was dizzy, nauseous, my heart felt like it was trying to escape my chest, and I spent three hours on the floor wondering if I was dying. I didn’t call anyone. I just lay there and cried. And then I realized-I’d ignored the warning because it looked like a generic sticker. That’s the problem. We’ve been trained to ignore small print. But small print? It’s the difference between living and being a statistic.
jesse chen
December 31, 2025 AT 07:20I really appreciate how this post breaks down the colors-red, yellow, blue-because I’ve always just assumed they were for pharmacy inventory. Also, the part about the teach-back method? That’s golden. I’ve used it with my grandma, and she actually remembers things now. She’ll say, ‘So if I eat grapefruit, I might pass out?’ and I’m like, ‘YES, THAT’S EXACTLY IT.’ She’s 78 and still learning. We all can.
Joanne Smith
December 31, 2025 AT 23:25Of course the pharmaceutical companies fought simplification. Why? Because if you make labels too clear, people might start asking why their $500 pill needs a 12-step warning just to not kill them. Meanwhile, the insert is printed in 6-point font on recycled paper. The real scandal isn’t patient ignorance-it’s corporate greed dressed up as ‘safety.’
Prasanthi Kontemukkala
January 1, 2026 AT 07:03I’m from India, and here, people often rely on the pharmacist’s word because they don’t trust the labels. But I’ve seen pharmacies give out the same pill in different colors with no explanation. This post reminded me how lucky we are to have even basic labeling systems. Maybe we need global standards-not just for language, but for how warnings are communicated. Everyone deserves to understand what they’re taking.
Michael Bond
January 1, 2026 AT 23:09QR codes on bottles? Genius. My dad can’t read small print. He scans the code, hears a voice explain it, and he’s good to go. No stress, no confusion.
Jody Kennedy
January 3, 2026 AT 11:46Stop throwing away those inserts! I keep mine in a folder labeled ‘My Health Arsenal.’ I’ve saved my life more than once by checking it before mixing meds. Also-yes, the grapefruit thing is real. I learned that the hard way. Now I carry a little card in my wallet: ‘NO GRAPEFRUIT. EVER.’
christian ebongue
January 4, 2026 AT 06:49pharmacists are overworked and underpaid so dont blame them if they dont explain everythng but also dont be lazy. ask. even if its awkward. i did and my doc changed my med. saved me from a stroke. its not hard.
Alex Ragen
January 4, 2026 AT 14:19One must ask: Is the problem truly the label-or the epistemological collapse of the modern subject, who has outsourced all agency to institutional authority, be it pharmaceutical, medical, or bureaucratic? The sticker is merely a symptom of a deeper alienation: we no longer trust our bodies, our intuition, or our capacity to discern. We wait for a color-coded icon to tell us when to die. And we call this progress.
Lori Anne Franklin
January 5, 2026 AT 13:26i never knew about the box warning thing!! i thought the sticker was all there was. now i keep the inserts in my purse like a bible. also i spelled everything wrong in this comment but you get the point 😘