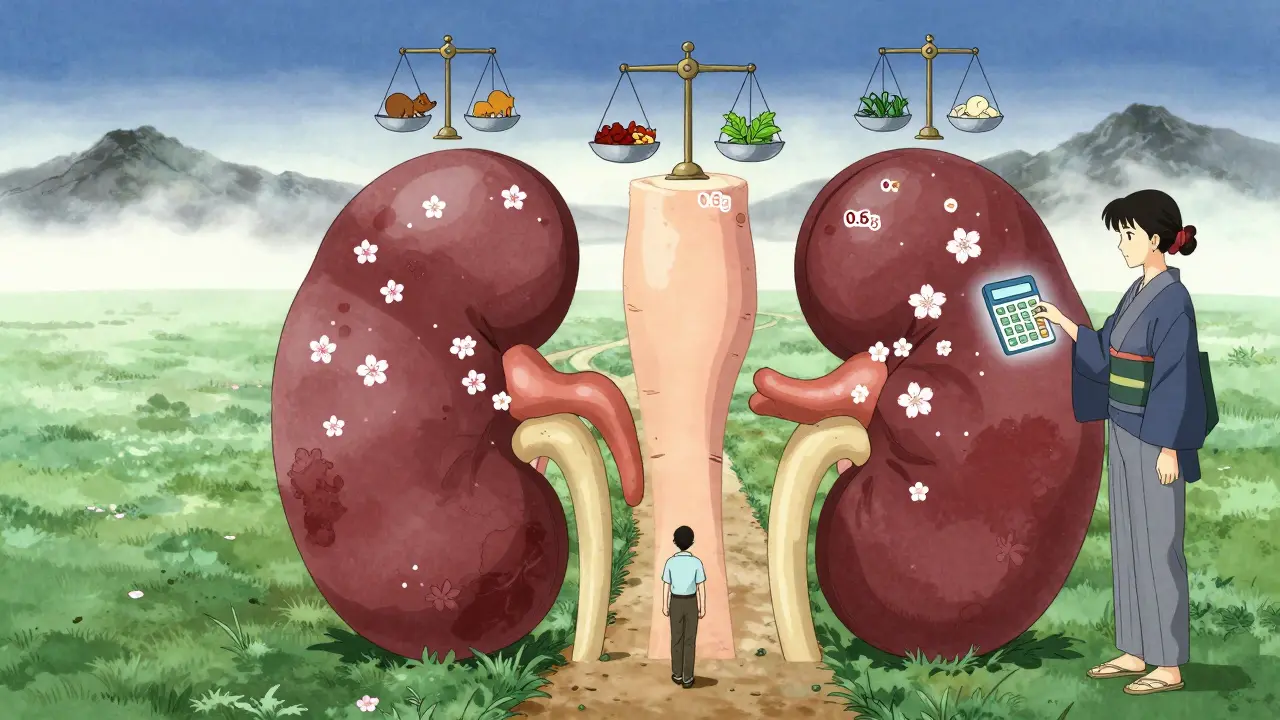
When your kidneys aren’t working well, what you eat matters more than you might think. Protein isn’t just about building muscle-it’s a major factor in how fast kidney disease progresses. Too much can overload your kidneys. Too little can leave you weak and malnourished. Finding the right balance isn’t one-size-fits-all. It changes depending on how far your kidney disease has advanced. This isn’t about cutting protein completely. It’s about getting the right amount of the right kind-and doing it safely.
What Protein Does (and Doesn’t Do) in Kidney Disease
Your kidneys filter waste from your blood. When you eat protein, your body breaks it down into nitrogen-based waste like urea. Healthy kidneys handle this easily. But when they’re damaged, that waste builds up. That’s why doctors have long recommended lowering protein intake in later stages of chronic kidney disease (CKD). The goal isn’t to starve you-it’s to slow the damage. Studies show that keeping protein intake within target ranges can delay the need for dialysis by 6 to 12 months.
But here’s the catch: protein restriction only works if you’re still getting enough calories and nutrients. If you cut protein too much, your body starts breaking down your own muscle. That’s called protein-energy wasting, and it affects up to half of people with stage 3b to 5 CKD. This isn’t just about feeling tired-it raises your risk of infection, hospitalization, and death.
Protein Targets by CKD Stage
Not all stages of kidney disease need the same protein limits. The guidelines have evolved, and now they’re more personalized than ever.
Stage 1 and 2 (GFR 60+): Your kidneys are still working fairly well. Most experts recommend sticking to 0.8 grams of protein per kilogram of ideal body weight. For someone who weighs 150 pounds (68 kg), that’s about 54 grams a day. This isn’t a strict limit-it’s a reminder to avoid high-protein diets. Eating 100+ grams daily isn’t helpful and might speed up kidney decline.
Stage 3a (GFR 45-59): Kidney function is starting to drop. Protein intake should be lowered to 0.6-0.8 g/kg/day. That’s 40-54 grams for a 150-pound person. At this stage, many people start noticing swelling, fatigue, or changes in urine. This is the best time to get help from a renal dietitian before things get harder to manage.
Stage 3b to 5 (GFR under 45): This is where protein restriction becomes more critical. The standard recommendation is 0.55-0.60 g/kg/day. For a 150-pound person, that’s 38-40 grams daily. But here’s where it gets tricky: if you’re older, frail, or have diabetes, these numbers might be too low. New research from 2024 found that older adults with early CKD who ate more protein (up to 0.8 g/kg) had lower death rates-not because protein was good for kidneys, but because they were less likely to become malnourished.
Diabetic patients with CKD need special care. The American Diabetes Association recommends 0.8-0.9 g/kg/day to protect both kidneys and blood sugar control. Going too low can cause dangerous drops in blood sugar or muscle loss.
Animal vs. Plant Protein: Which Is Better?
Not all protein is created equal when it comes to kidney health. The source matters just as much as the amount.
Animal proteins-like meat, eggs, dairy, and seafood-contain all the essential amino acids your body needs. They’re called “high biological value” proteins. But they also produce more waste. One gram of animal protein generates about 20-30% more urea and phosphate than plant protein. They also create more advanced glycation end products (AGEs), which cause inflammation and oxidative stress in people with kidney disease.
Plant proteins-beans, lentils, tofu, nuts, and whole grains-are gentler on the kidneys. A 2021 study showed that replacing just 30% of animal protein with plant protein lowered the risk of CKD worsening by 14% and cut death risk by 11%. That’s a big deal.
But plant proteins have a downside: they’re often missing key amino acids like lysine and methionine. If you rely only on plants, you might not get enough protein quality to maintain muscle. The solution? Combine sources. Eat rice with beans. Add soy products like tofu or tempeh. Use pea protein powders designed for kidney patients. The goal is to get at least half your daily protein from high-quality sources, whether animal or plant-based.

Why So Many People Struggle
Even with clear guidelines, most people find it hard to stick to low-protein diets. A 2024 survey from the American Kidney Fund found that 74% of patients felt constantly hungry after cutting protein. 62% reported muscle weakness. 58% said they avoided social meals because they couldn’t eat what everyone else was having.
Tracking protein is another hurdle. Most people don’t realize how much protein is in mixed dishes-like pasta with meat sauce, stir-fries, or even sandwiches. One cup of cooked lentils has 18 grams. One egg has 6. One slice of bread has 3-4. Add it all up, and you hit your limit before lunch.
And here’s the reality: only 35% of nephrologists refer their patients to renal dietitians, even though guidelines say they should. That means most people are left guessing. But those who work with a dietitian? 82% say they feel more in control and have better quality of life.
How to Make It Work
Managing protein in CKD isn’t about perfection. It’s about practical steps.
- Use a protein calculator. The National Kidney Foundation’s app has been downloaded nearly 50,000 times. It lets you log meals and see your daily protein total in real time.
- Meal prep. Cook kidney-friendly meals in batches-like vegetable soups with egg whites, tofu scrambles, or grain bowls with small portions of chicken. Freeze them. You won’t be tempted to reach for high-protein fast food.
- Choose low-potassium, low-phosphorus options. If you’re in stage 4 or 5, you’re also watching potassium and phosphorus. Swap potatoes for cabbage. Use white rice instead of brown. Pick fresh fruit over dried.
- Consider keto acid supplements. These are prescription products (like Ketosteril) that provide essential amino acids without the nitrogen waste. Used in 15% of European stage 4-5 patients, they help you stay on low-protein diets without losing muscle.
- Work with a renal dietitian. Even one 90-minute session can change your entire approach. Follow-ups every 4-6 weeks help adjust your plan as your condition changes.
There’s also new tech on the horizon. The NIH-funded PRECISE-CKD trial is testing whether personalized protein targets-based on your body’s actual urea production-are better than the standard weight-based formulas. Early results suggest some people might need more protein than others, even in late-stage CKD.
The Bigger Picture
The future of renal nutrition isn’t just about cutting protein. It’s about smart choices. Experts now agree: quality matters more than quantity. A plant-forward, low-sodium, low-phosphorus diet with enough high-quality protein can do more than slow kidney decline-it can improve energy, mood, and survival.
By 2030, most nephrologists expect individualized protein plans to be standard care. That means your diet won’t be based on a chart in a textbook. It’ll be built around your age, muscle mass, activity level, diabetes status, and even your food preferences.
Don’t try to do this alone. If you have CKD, ask your doctor for a referral to a renal dietitian. Use the tools available. Track your meals. Learn what’s in your food. The goal isn’t to eat less-it’s to eat smarter.
How much protein should I eat if I have stage 3 CKD?
For stage 3 CKD (GFR 30-59 mL/min), aim for 0.6 to 0.8 grams of protein per kilogram of ideal body weight per day. For a 150-pound person, that’s about 40-54 grams daily. If you’re older, diabetic, or losing weight, your dietitian may recommend the higher end of this range to prevent muscle loss.
Can I eat beans and lentils with kidney disease?
Yes-but with caution. Beans and lentils are excellent plant-based proteins that produce less waste than meat. However, they’re high in potassium and phosphorus. If you’re in stage 4 or 5, soak them overnight, rinse well, and cook in fresh water to reduce minerals. Limit portions to ½ cup cooked per meal. Pair them with low-potassium foods like white rice or cabbage.
Why do I feel weak on a low-protein diet?
You may not be getting enough calories or high-quality protein. Feeling weak is often a sign of protein-energy wasting, which affects up to half of late-stage CKD patients. Talk to your dietitian about adding high-biological-value proteins like egg whites, tofu, or keto acid supplements. Also, make sure you’re eating enough carbs and healthy fats to fuel your body.
Is a vegan diet safe for kidney disease?
A well-planned vegan diet can be safe and even beneficial for early-stage CKD. Plant proteins reduce kidney stress and lower inflammation. But you must combine sources (like rice + beans) to get all essential amino acids. Monitor potassium and phosphorus closely. Avoid high-potassium foods like spinach, bananas, and potatoes. Work with a renal dietitian to avoid nutrient gaps.
Do I need protein supplements?
Most people don’t need regular protein powders-they’re often too high in phosphorus and potassium. Instead, renal-specific supplements like keto acid analogues (e.g., Ketosteril) are prescribed to patients on very low-protein diets. These provide amino acids without nitrogen waste. Only use them if your doctor or dietitian recommends them.
Can protein restriction delay dialysis?
Yes. The 2022 Cochrane Review found that sticking to a low-protein diet (0.6-0.8 g/kg/day) reduced the risk of reaching end-stage kidney disease by 31% over 2-4 years. That means many people can delay dialysis by 6 to 12 months. But this only works with consistent adherence and proper calorie intake.
What to Do Next
If you’re managing CKD, start with one step: ask your nephrologist for a referral to a renal dietitian. Don’t wait until you’re in stage 4 or 5. The earlier you get support, the easier it is to adapt.
Download the National Kidney Foundation’s Protein Target Calculator. Try one kidney-friendly recipe from Kidney Kitchen this week. Track your protein for three days using an app like MyFitnessPal with a renal database.
This isn’t a diet you give up on. It’s a lifestyle you learn. With the right tools and support, you can eat well, feel better, and protect your kidneys-for as long as possible.

Kitty Price
December 16, 2025 AT 20:58Ron Williams
December 17, 2025 AT 09:51Joanna Ebizie
December 17, 2025 AT 15:19Randolph Rickman
December 18, 2025 AT 11:58Hadi Santoso
December 20, 2025 AT 03:16Dylan Smith
December 20, 2025 AT 10:07Elizabeth Bauman
December 20, 2025 AT 19:12Billy Poling
December 22, 2025 AT 13:52Mike Smith
December 23, 2025 AT 16:48Colleen Bigelow
December 23, 2025 AT 23:28Aditya Kumar
December 24, 2025 AT 17:52Arun ana
December 25, 2025 AT 11:24