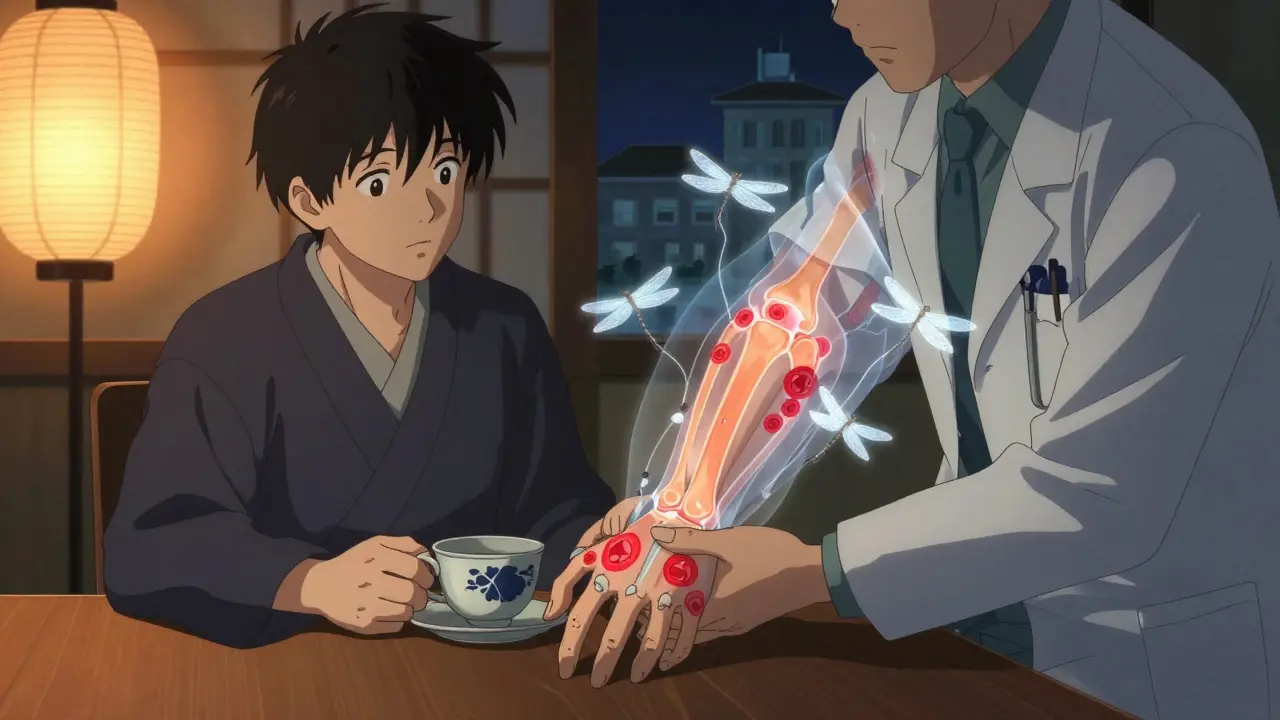
When your body turns against itself, it doesn’t just hurt-it changes everything. Rheumatoid arthritis (RA) isn’t just stiff joints or aching hands. It’s an autoimmune storm inside your body, where your immune system mistakes your own joint lining for an invader and starts tearing it down. This isn’t wear and tear like osteoarthritis. This is war-and it starts quietly, often in the small joints of your fingers or toes, before spreading like wildfire.
What Makes Rheumatoid Arthritis Different?
RA doesn’t show up overnight. It creeps in over weeks or months. You might notice your knuckles feel swollen, your morning stiffness lasts longer than usual-maybe 45 minutes or more-and it doesn’t get better with coffee or stretching. Unlike osteoarthritis, which comes from aging or injury, RA is driven by your immune system. It sends antibodies straight to the synovium, the soft tissue lining your joints. That’s where the inflammation begins, and from there, it eats away at cartilage, then bone.
Doctors look for three key signs: symmetric joint pain (both wrists, both knees), morning stiffness lasting half an hour or longer, and symptoms that stick around for six weeks or more. Blood tests check for rheumatoid factor (RF) and anti-CCP antibodies-markers that tell if your immune system is on the attack. X-rays and ultrasounds show early swelling, then later, bone erosion. About 10-15% of people with RA also develop Sjögren’s syndrome, where eyes and mouth dry out because the immune system attacks moisture-producing glands.
And it’s not just joints. RA can affect your lungs, heart, blood vessels, and even your skin. Rheumatoid nodules-firm lumps under the skin near elbows or fingers-are common. People with RA have a higher risk of heart disease and anemia. The disease doesn’t just limit movement; it steals energy, sleep, and confidence.
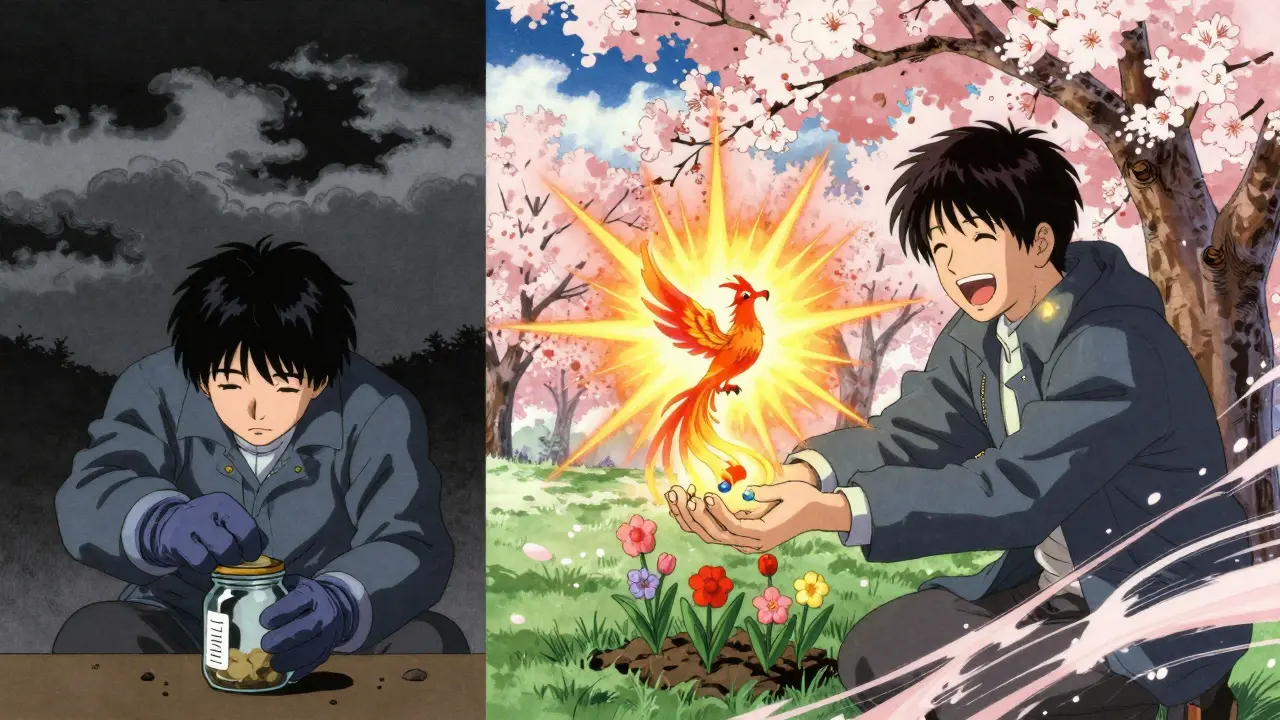
Why Early Treatment Changes Everything
There’s a narrow window-just three to six months after symptoms start-where you can stop RA from doing permanent damage. After that, joint erosion becomes irreversible. That’s why experts say: treat fast, treat hard. Delaying treatment isn’t just risky-it’s costly. Every month you wait increases your chance of needing joint replacements, losing work, or becoming dependent on others for daily tasks.
Studies show that people who start aggressive treatment within the first six months are twice as likely to reach remission. The goal isn’t just to feel better today-it’s to be able to hold your grandchild, type on a keyboard, or button your shirt five years from now. That’s why the American College of Rheumatology and EULAR guidelines push for a “treat-to-target” approach: set a clear goal (remission or low disease activity), check your progress every 1-3 months, and adjust meds until you get there.
First-Line Treatment: Methotrexate and Beyond
Most RA patients start with methotrexate. It’s old, it’s cheap, and it works. About 68% of new prescriptions in 2023 were for methotrexate. It’s a disease-modifying antirheumatic drug (DMARD) that slows the immune system’s attack. But it’s not perfect. Side effects include nausea, fatigue, and liver stress. About 30% of people stop taking it within a year because it doesn’t work well enough-or they can’t tolerate it.
That’s where biologics come in. These aren’t pills. They’re targeted therapies designed to block specific parts of the immune system that fuel inflammation. Unlike methotrexate, which acts broadly, biologics are like precision missiles. They don’t shut down your whole immune system-they just silence the parts causing the damage.
The Biologic Arsenal: What’s Available Now?
There are four main types of biologics used for RA today:
- TNF inhibitors (adalimumab, etanercept, infliximab): These block tumor necrosis factor, a major inflammation driver. They’re the most prescribed-making up 55% of all biologic use. Humira (adalimumab) is the most common, with many patients reporting big improvements in pain and mobility.
- IL-6 inhibitors (tocilizumab): These stop interleukin-6, another key inflammatory signal. One patient in the Arthritis Foundation’s community said after starting tocilizumab, she played piano again for the first time in five years.
- B-cell inhibitors (rituximab): These remove B-cells, the immune cells that produce harmful antibodies. Often used when TNF blockers fail.
- T-cell costimulation blockers (abatacept): These prevent T-cells from activating the immune response. Useful for patients who can’t take TNF inhibitors.
Combined with methotrexate, biologics reduce disease activity by 50% or more in about 60% of patients. Alone, methotrexate helps only 40%. That’s a big jump. But they’re not magic. About 30% of patients don’t respond well to their first biologic. That’s why doctors often try different ones-switching isn’t failure, it’s strategy.
The Real Costs: Money, Side Effects, and Daily Life
Biologics are expensive. Annual costs range from $15,000 to $60,000. Even with insurance, co-pays can hit $500 a month. A 2023 Arthritis Foundation survey found 41% of patients skipped doses or stopped treatment because of cost. That’s not just a financial burden-it’s a health crisis.
Then there are side effects. Biologics suppress parts of your immune system. That means higher risk of serious infections: pneumonia, tuberculosis, even sepsis. Studies show a 1.5 to 2 times higher infection risk compared to traditional DMARDs. That’s why every patient gets screened for TB before starting. You can’t get live vaccines while on biologics. If you get a fever, you call your doctor-not wait it out.
Some patients report injection site reactions-redness, itching, swelling. Others feel fatigued or develop rashes. A small number face increased lymphoma risk, though the absolute risk remains low. The FDA requires all biologics to have a Risk Evaluation and Mitigation Strategy (REMS) program. That means you and your doctor must complete training on infection signs before you can get a prescription.
What’s New in 2025?
The RA treatment landscape is changing fast. In September 2023, the first biosimilar to Humira (adalimumab-adaz) got FDA approval. Biosimilars are nearly identical to the original biologic but cost 15-20% less. More are coming. In January 2024, upadacitinib (Rinvoq), a JAK inhibitor, got expanded approval for early RA. It’s a pill, not an injection, and it works quickly.
Researchers are now testing selective TYK2 inhibitors like deucravacitinib-new drugs that target inflammation more precisely with fewer side effects. Phase 3 trials are ongoing, with potential approval by 2026. Meanwhile, genetic testing is getting better. A 2023 study in Nature Medicine used biomarkers to predict methotrexate response with 85% accuracy. Imagine knowing before you start whether a drug will work for you.
Living With RA: Beyond the Medication
Medication is only half the battle. The other half is lifestyle. Regular movement matters. The CDC recommends 150 minutes of moderate exercise a week-walking, swimming, cycling. Strength training helps protect joints. Losing 5-10% of body weight can cut disease activity by 20-30% in overweight patients.
Self-management tools help too. Apps like MyRA let you track symptoms, meds, and flares. The Arthritis Foundation’s Live Yes! Network offers peer support and workshops. CDC-backed self-management classes reduce pain by 20% in six months. And mental health? Crucial. Depression and anxiety are common in RA patients. Talking to a counselor isn’t optional-it’s part of treatment.
On Reddit’s r/rheumatoidarthritis community, people share real stories: one man couldn’t open jars for years, then started swimming and regained grip strength. A woman stopped wearing gloves in winter because her hands didn’t ache anymore after switching to rituximab. These aren’t outliers-they’re proof that progress is possible.
What Comes Next?
By 2030, the number of Americans with RA is expected to rise to 1.7 million. Rural patients still face barriers-30% less likely to get biologics than those in cities. Access isn’t just about money. It’s about specialists. Not every town has a rheumatologist. Telehealth helps, but it’s not a full fix.
The future is personalized. We’re moving away from trial-and-error treatment toward matching the right drug to the right person based on genetics, biomarkers, and disease patterns. The goal? No more flares. No more joint damage. No more losing years of your life to pain.
RA is chronic. But it doesn’t have to be crippling. With early diagnosis, the right combination of meds, and strong support, most people don’t just survive-they live. Fully. Freely. Without waiting for the next flare to hit.
Can rheumatoid arthritis be cured?
There is no cure for rheumatoid arthritis yet. But with early, aggressive treatment-especially using biologics combined with methotrexate-many people achieve remission, meaning symptoms disappear and disease activity drops to near zero. Remission isn’t the same as a cure; the immune system still has the potential to flare again. That’s why ongoing monitoring and treatment are essential, even when you feel fine.
How do I know if a biologic is working for me?
You’ll know if your pain and stiffness decrease, your joints feel less swollen, and you regain daily function-like opening jars, typing, or walking without help. Doctors use tools like the DAS28 score, which measures joint tenderness, swelling, and blood markers of inflammation. A drop of 1.2 or more in this score after 3-6 months usually means the treatment is working. If you’re not improving, your rheumatologist may switch you to another biologic or add a JAK inhibitor.
Are biologics safe for long-term use?
Biologics have been used for over 25 years, and long-term safety data is strong. Most people tolerate them well for years. But risks include serious infections, reactivation of latent TB, and a small increase in lymphoma risk. Regular check-ups, blood tests, and screenings are critical. Never stop a biologic suddenly-this can cause a dangerous flare. Always work with your rheumatologist to manage risks and adjust treatment over time.
Can I take biologics if I have other health conditions?
It depends. If you have active infections, hepatitis B, heart failure, or multiple sclerosis, some biologics may not be safe. TNF inhibitors, for example, are avoided in people with heart failure or demyelinating diseases. Your doctor will screen you for these conditions before starting. If you have diabetes, COPD, or a history of cancer, your team will weigh risks carefully. Many people with controlled conditions still use biologics successfully-just not all types.
What if I can’t afford biologics?
You’re not alone. Many drugmakers offer patient assistance programs that cut costs to $0 or $50 a month. Biosimilars are now available and can save 15-20%. Some nonprofits, like the Arthritis Foundation, help with co-pay aid. Talk to your rheumatologist’s office-they have financial counselors who specialize in RA. Don’t skip doses because of cost. There are options. You just need to ask.
Do I still need physical therapy if I’m on biologics?
Yes. Medication stops inflammation, but therapy rebuilds strength and mobility. RA can cause muscle loss and joint stiffness even when inflammation is under control. A physical therapist can design exercises to protect your joints, improve range of motion, and teach you joint-saving techniques for daily tasks. Many people report better outcomes when they combine biologics with regular PT. It’s not optional-it’s part of the treatment plan.

Lisa Davies
December 15, 2025 AT 18:34Just wanted to say this post gave me chills. I was diagnosed with RA at 29, and no one told me it could affect my lungs until I started coughing up blood. Biologics saved my life-but I had to fight my insurance for 11 months. You’re not alone if you’re scared. Keep going. 💪❤️
RONALD Randolph
December 16, 2025 AT 19:16Let me be perfectly clear: the American healthcare system is a disgrace. A 60,000-dollar-per-year drug-while people die waiting for Medicaid approval-is not medicine. It’s extortion. And the FDA? Complicit. Biosimilars? A Band-Aid on a severed artery. We need universal healthcare-or this epidemic will bury us all.
Christina Bischof
December 17, 2025 AT 18:09My mom’s been on Humira for 8 years. She still knits. Still gardens. Still drives to the lake. It’s not perfect-but it’s enough. I just wish more people knew that remission doesn’t mean ‘cured.’ It means ‘alive, and trying.’
Michelle M
December 18, 2025 AT 00:03There’s something quiet about chronic illness that no one talks about. It’s not the pain-it’s the grief. The grief for the person you were before the diagnosis. The person who could run without thinking. The person who didn’t count calories before every medication. You don’t have to ‘stay positive’ to be brave. Sometimes, just showing up is the revolution.
Nupur Vimal
December 18, 2025 AT 18:19You all talk like biologics are magic. In India, most people can't even get methotrexate. RA is a rich person's disease. Your biologics won't save the global south. Stop acting like this is about health-it's about capitalism.
Cassie Henriques
December 18, 2025 AT 23:51Just got my DAS28 back-down to 1.8 after switching to Rinvoq. My CRP was 12 last month; now it’s 0.8. The fatigue is still real, but I can finally hold my coffee without shaking. JAK inhibitors are a game-changer for TNF non-responders. Also, the pill form? Absolute luxury. No more needles before brunch.
Benjamin Glover
December 20, 2025 AT 22:21Biologics are overrated. In the UK, we manage with NSAIDs and physio. Your American pharmaceutical addiction is pathological. You’re treating symptoms, not discipline.
John Samuel
December 21, 2025 AT 07:02Imagine a world where your immune system doesn’t betray you. Where your joints don’t scream at dawn. Where you wake up and don’t have to calculate the cost of movement. That’s not fantasy-it’s the future we’re building with TYK2 inhibitors, biomarkers, and patient-driven research. We’re not just managing RA anymore. We’re rewriting its narrative. One data point, one dose, one reclaimed morning at a time.
Jake Sinatra
December 22, 2025 AT 15:59The notion that early intervention is critical is not merely clinical-it’s existential. The window of opportunity is not metaphorical; it is quantifiable, measurable, and unforgiving. Delaying treatment is not an option; it is a calculated risk with irreversible consequences. The data is unequivocal. Action must precede regret.
Mike Nordby
December 24, 2025 AT 12:41Just had my first telehealth rheum consult. The doctor asked if I’ve tried PT. I said no-too expensive. She sent me a link to CDC’s free self-management program. I started yesterday. Two weeks in: I can button my shirt again. Medication helps. But movement? That’s the real medicine.