Medication Splitting Safety Checker
Check Your Medication Safety
Enter your medication name to see if it can be safely split or if dose splitting is recommended.
Many people split their pills to save money or ease side effects-thinking it’s just a simple trick. But what if splitting your pill could make things worse? The truth is, not all pills are meant to be split. Some do better when taken whole. Others need careful timing, not just a cut in half. The goal isn’t to break a tablet-it’s to manage how much drug hits your bloodstream at once. That’s where dose splitting comes in: taking the same total daily amount, but in smaller, more frequent doses to smooth out the spikes.
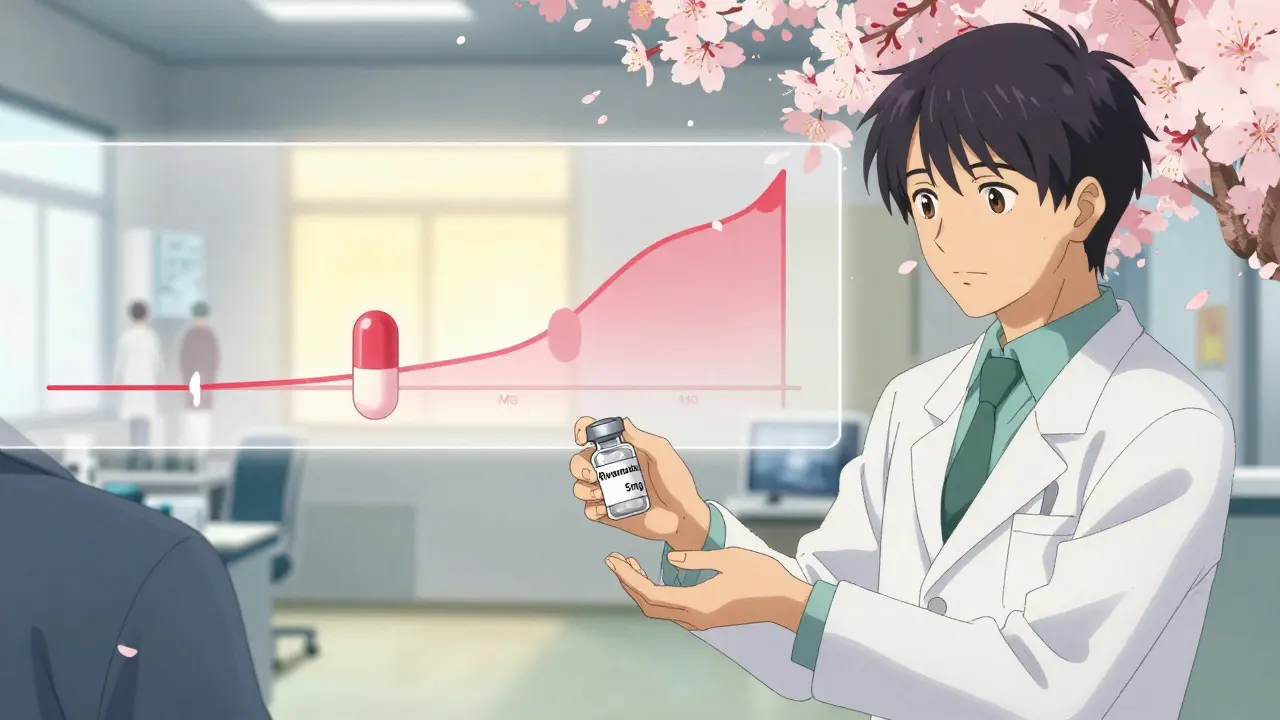
Why Peak Concentrations Matter
When you swallow a pill, your body absorbs it, and drug levels rise in your blood. That’s the peak. Too high, and you get side effects-dizziness, nausea, headaches, or worse. Too low, and the medicine doesn’t work. For some drugs, even a small spike can trigger problems. Take digoxin, used for heart rhythm issues. Its safe range is tiny: 0.5 to 2.0 nanograms per milliliter. Go above that, and you risk dangerous heart rhythms. Splitting a 0.25mg dose into two 0.125mg doses taken 12 hours apart keeps levels steadier. That’s dose splitting. It’s not about cutting a pill-it’s about changing when you take it.Not All Pills Are Created Equal
You can’t just split any pill and expect the same result. Immediate-release pills, like lisinopril for blood pressure, are designed to dissolve quickly. Splitting the daily dose-say, 10mg twice a day instead of 20mg once-can lower the peak by about 25%. That means less cough, less dizziness, and fewer people stopping the medicine because it felt awful. But extended-release pills? Those are different. They’re built to release drug slowly over hours. If you split a 40mg extended-release tablet of tramadol or felodipine, you’re breaking the coating or matrix that controls release. Instead of a slow drip, you get a rush. One study found that splitting enteric-coated tablets increased early dissolution by 30-50%. That’s not safer-it’s riskier. The Australian Prescriber warns that this can lead to unpredictable spikes, especially with drugs that have narrow therapeutic windows.Which Drugs Can Be Split Safely?
There’s a short list of medications where dose splitting actually helps:- Immediate-release metformin: Patients report fewer stomach issues when taking 500mg four times a day instead of 1000mg twice.
- Immediate-release lisinopril: Smoother blood pressure control, less dry cough.
- Immediate-release stimulants (like methylphenidate): Less jitteriness when split into morning and early afternoon doses.
- Immediate-release opioids (like oxycodone IR): Lower peak reduces nausea and drowsiness.
- Immediate-release antipsychotics: Reduced sedation when split into smaller, more frequent doses.
Drugs You Should Never Split
Some pills are dangerous to split, even if they have a score line. The FDA has logged over 1,200 adverse events between 2015 and 2020 from improper splitting. The worst offenders:- Warfarin: A slight dose change can cause bleeding or clots. Even 5% variation in split tablets can push INR levels out of range.
- Extended-release oxycodone: Splitting releases the full dose at once-risk of overdose.
- Enteric-coated aspirin: The coating protects your stomach. Break it, and you get ulcers.
- Immunosuppressants (like cyclosporine): Tiny changes can trigger organ rejection.
- Chemotherapy drugs: Precision matters. No room for error.
Tablet Splitting vs. Dose Splitting
This is where people get confused. Tablet splitting means cutting a pill in half to take two doses. Dose splitting means taking the same total daily amount in smaller, more frequent doses-without necessarily cutting the pill. For example:- Tablet splitting: You buy 20mg lisinopril tablets, cut them in half, and take one half in the morning and one at night. But if the tablet isn’t scored evenly, you might get 12mg one day and 8mg the next.
- Dose splitting: Your doctor prescribes 10mg lisinopril tablets and tells you to take one in the morning and one at night. No cutting. No guesswork. Just two 10mg doses.
How to Do It Right
If your doctor says dose splitting is right for you, here’s how to do it safely:- Ask first. Never split a pill without talking to your pharmacist or prescriber. They’ll check the formulation, half-life, and therapeutic index.
- Use a pill splitter. Not a knife. Not scissors. A dedicated, clean pill splitter reduces variation from 25% to under 8%.
- Split only immediate-release pills. If it says “ER,” “XR,” “SR,” “CR,” or “extended-release,” leave it whole.
- Store split tablets properly. Keep them in their original bottle, away from moisture, and use within a week. Moisture degrades some drugs.
- Monitor for changes. If you’re on warfarin, check INR within 7 days. If you’re on blood pressure meds, track your readings. Side effects should improve-not get worse.
The Cost Trap
Many people split pills to save money. A 80mg atorvastatin tablet costs $20. Two 40mg tablets cost $30. Splitting saves $10 a month. But if you split a pill that shouldn’t be split, you could end up in the ER. The FDA estimates that inappropriate splitting adds $12.3 billion in avoidable healthcare costs each year in the U.S. Meanwhile, drugmakers are responding: Pfizer now sells 5mg and 10mg rivaroxaban tablets, which cut splitting attempts by 78%. Lower-dose options are becoming more common. Ask your pharmacist: Is there a lower-dose version available? It might be safer-and not much more expensive.What’s Next?
The NIH is running a trial called SPLIT-PEAK (NCT05521034) to see if splitting venlafaxine doses reduces nausea without losing effectiveness. Early results are promising. Meanwhile, seven pharmaceutical companies are working on “smart” tablets with engineered split points that preserve extended-release properties. But until those are widely available, stick to the basics: if your drug isn’t on the safe list, don’t split it. If you’re unsure, ask. Your pharmacist has the answers.Side effects aren’t something you just have to live with. But fixing them isn’t always about cutting a pill in half. Sometimes, it’s about changing when you take it-and never guessing.
Can I split my pill to save money?
You can, but only if it’s safe. Immediate-release pills like lisinopril or metformin can often be split without risk. But extended-release, enteric-coated, or narrow-therapeutic-index drugs like warfarin or oxycodone ER should never be split. Always check with your pharmacist first. A $10 monthly saving isn’t worth an ER visit.
Does splitting a pill reduce side effects?
It can-but only for certain drugs. For medications with short half-lives and concentration-dependent side effects (like nausea from metformin or dizziness from stimulants), splitting the daily dose into smaller, more frequent doses can smooth out blood levels and reduce peaks. This lowers side effects without losing effectiveness. But for other drugs, splitting creates dangerous spikes.
What’s the difference between dose splitting and tablet splitting?
Tablet splitting means physically cutting a pill in half and taking both halves. Dose splitting means taking the same total daily amount in smaller doses spread throughout the day-usually by using lower-dose tablets. For example: taking two 10mg tablets (dose splitting) vs. cutting one 20mg tablet in half (tablet splitting). The first is more precise and safer.
Are scored pills always safe to split?
No. A score line doesn’t mean it’s safe. Some scored tablets are designed for visual alignment, not accurate splitting. Extended-release or enteric-coated pills may have score lines for manufacturing reasons, not patient use. Always check the drug’s prescribing information or ask your pharmacist. About 22% of scored tablets in Europe carry a "do not split" warning due to content variability.
How do I know if my medication has a narrow therapeutic index?
Drugs with a narrow therapeutic index have a very small range between an effective dose and a toxic one. Common examples: warfarin (INR 2-3), digoxin (0.5-2.0 ng/mL), lithium, phenytoin, and cyclosporine. If your doctor says your drug requires regular blood tests to monitor levels, it likely has a narrow therapeutic index. Don’t split these unless explicitly instructed by your healthcare provider.
Can I split my pill with a knife or scissors?
It’s not recommended. A knife or scissors can crush the tablet, create uneven pieces, or leave residue. Studies show this increases dose variability to 25% or more. Use a dedicated pill splitter-it costs less than $10 and cuts pills within 5-8% accuracy. It’s a small investment for safety.
What should I do if I accidentally split a pill that shouldn’t be split?
Stop taking it. Contact your pharmacist or doctor immediately. If you took an extended-release opioid, stimulant, or anticoagulant, seek medical advice right away. Watch for signs like dizziness, irregular heartbeat, bleeding, or severe nausea. Don’t wait for symptoms to appear. Even one incorrect split can be dangerous.
Is dose splitting covered by insurance?
Insurance doesn’t cover the act of splitting-it covers the medication. If your doctor prescribes a lower-dose tablet instead of having you split a higher one, your insurance will cover the lower-dose version the same way. Sometimes, lower-dose versions cost less than splitting higher ones. Ask your pharmacist about cost-effective alternatives.
If you’re managing side effects from your medication, don’t guess. Talk to your pharmacist. They know which pills can be split, which can’t, and what alternatives exist. A simple conversation could prevent a hospital visit.
Ted Conerly
January 10, 2026 AT 11:56Splitting pills to save money is a classic case of penny-wise and pound-foolish. I've seen patients end up in the ER because they thought cutting a 40mg extended-release tablet in half was harmless. It's not. The science here is clear: dose splitting with immediate-release formulations works. Tablet splitting? Not so much. Always check with your pharmacist. A $10 monthly save isn't worth a cardiac event.
McCarthy Halverson
January 10, 2026 AT 17:08Don't split anything without asking. Pill splitters cost ten bucks. ER visits cost thousands.
Mario Bros
January 12, 2026 AT 04:22My grandma used to split her metformin with a knife and swore it helped her stomach. Turns out she was just lucky. Now she uses the 500mg tablets and never complains. Don't be like grandma. Get the right dose. It's not that hard.
Jake Nunez
January 12, 2026 AT 13:40Just came back from a trip to Mexico and saw people splitting warfarin like it was candy. No one there checks INR. No one even knows what INR means. This isn't just a US problem-it's a global blind spot. Education needs to be part of the prescription, not an afterthought.
Christine Milne
January 14, 2026 AT 11:13It's absurd that we're even having this conversation. In my country, we don't let laypeople handle pharmaceutical dosing like it's a DIY project. The FDA's own data shows over 1,200 adverse events from improper splitting. This isn't innovation-it's negligence dressed up as frugality. Someone should be held accountable.
Bradford Beardall
January 14, 2026 AT 19:28Wait, so if I'm on immediate-release oxycodone and I split the dose into three 5mg doses instead of two 7.5mg ones, would that actually reduce nausea? Or am I just overthinking it? I've been having bad mornings since I switched from the ER version. Any data on that?
Michael Marchio
January 15, 2026 AT 15:04You know what's really dangerous? People reading this and thinking they now know enough to make medical decisions based on a Reddit post. I've seen this exact scenario play out a dozen times. Someone finds a blog, thinks they're smart, starts splitting pills, then shows up at the clinic three weeks later with a drug level that's off the charts. And then they wonder why their doctor won't trust them anymore. It's not that complicated. If the label says 'extended-release,' don't touch it. If your pharmacist says no, don't argue. Your life isn't a lab experiment.
Dwayne Dickson
January 16, 2026 AT 05:49While the clinical rationale for dose splitting in immediate-release formulations is well-supported by pharmacokinetic principles-particularly in drugs with short half-lives and concentration-dependent adverse effect profiles-it is imperative to distinguish between pharmacological intent and patient self-optimization. The notion that pill splitting equates to therapeutic optimization is a dangerous heuristic, especially when compounded by socioeconomic pressures. The 2020 UBC study demonstrating up to 40% variability in unscored tablets underscores the non-trivial risk of dose inaccuracy, which in turn introduces nonlinear pharmacodynamic consequences. Furthermore, the economic argument for splitting is increasingly obsolete, as evidenced by Pfizer’s introduction of lower-dose rivaroxaban formulations reducing splitting attempts by 78%. The future lies not in manual fragmentation but in precision dosing engineered into the formulation itself. Until then, the burden of safety rests not on the patient’s scissors, but on the prescriber’s guidance and the pharmacist’s verification. A simple consultation may prevent a lifetime of complications.