When you start taking a statin to lower your cholesterol, you expect to protect your heart-not end up with aching legs, weak arms, or constant fatigue. But for many people, that’s exactly what happens. Statin-induced muscle pain isn’t just a minor annoyance. It’s a real, measurable condition that can range from mild discomfort to life-altering muscle damage. And it’s more common than most doctors admit.
What’s Really Going On When Statins Hurt Your Muscles?
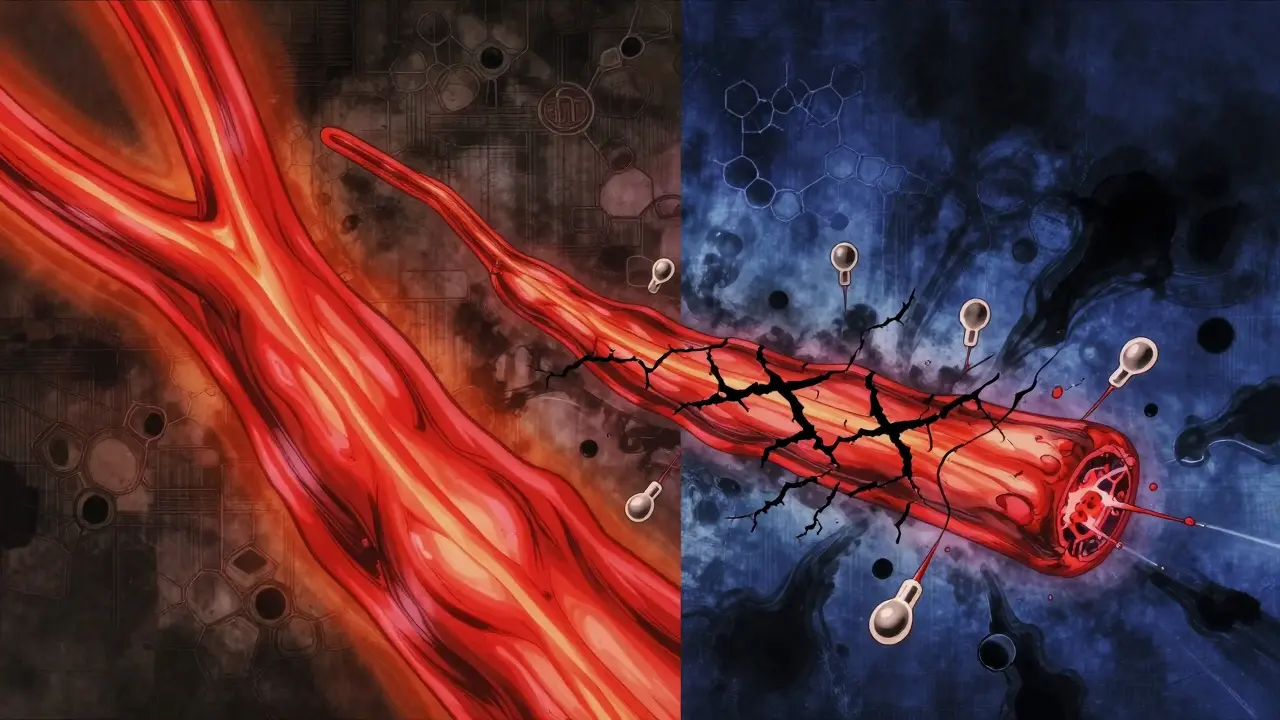
Statins work by blocking an enzyme called HMG-CoA reductase. That’s how they lower LDL cholesterol. But that same enzyme is also critical for making other compounds your muscles need-like coenzyme Q10 (CoQ10), which powers your muscle cells’ energy factories. When statins cut CoQ10 production by up to 40%, your muscles start running on empty. That’s why you feel tired, stiff, or sore, even if you haven’t changed your routine. But it’s not just about energy. Statins also mess with proteins that help control calcium levels inside muscle cells. When calcium leaks out of control, it triggers enzymes that eat away at muscle tissue. Add to that an increase in the body’s natural muscle-wasting system-the ubiquitin-proteasome pathway-and you’ve got a perfect storm for muscle breakdown.Myalgia vs. Myositis: Not All Muscle Pain Is the Same
Not every ache is the same. Statin-related muscle problems fall into three main buckets:- Myalgia: Muscle pain without any rise in creatine kinase (CK), a marker of muscle damage. This affects 10-29% of users. You feel sore, maybe crampy, but your blood tests look normal. It often goes away within a week or two after stopping the statin.
- Myositis: Inflammation in the muscle with CK levels 10 to 40 times higher than normal. This isn’t just soreness-it’s actual muscle injury. You might notice weakness climbing stairs or lifting your arms. Blood tests confirm it.
- Immune-mediated necrotizing myopathy (IMNM): Also called statin-associated autoimmune myopathy (SAAM). This is rare-only 2-3 cases per 100,000 statin users-but it’s serious. Your body starts attacking its own muscle tissue because it mistakes the HMG-CoA enzyme for a threat. CK levels often soar above 2,000 IU/L (normal is 30-200). Symptoms get worse even after you stop the statin, and recovery can take months or years without treatment.
Here’s the catch: most doctors test for CK and assume if it’s normal, you’re fine. But in SAAM, CK can be normal at first, then spike later. And muscle pain that lingers beyond two weeks? That’s not normal. That’s a red flag.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to develop statin muscle problems:- People over 50
- Those taking high-dose statins (like 80 mg atorvastatin)
- Patients on other meds that interact with statins-like amiodarone, fibrates, or certain antibiotics-can see statin levels jump 300-500%
- African Americans have nearly double the risk compared to Caucasians, likely due to a gene variant (SLCO1B1) that affects how statins enter the liver
- People with low vitamin D or thyroid problems
And genetics matter. If you carry the rs4149056 SNP, your risk of muscle pain on simvastatin jumps from 0.6% to 1.4%. That’s not a huge number, but for someone already feeling weak, it’s enough to change everything.
Why Diagnosis Takes So Long
Many patients spend months being told they have fibromyalgia, chronic fatigue, or just “getting older.” One Reddit user shared that after 18 months of progressive weakness following atorvastatin use, he finally got diagnosed with SAAM-and needed six months of IVIG therapy to start improving. On the Myositis Support and Understanding forum, 68% of SAAM patients reported being misdiagnosed for over a year. Why? Because the symptoms mimic other conditions. And most GPs don’t test for anti-HMGCR antibodies unless the case is obvious. The European Atherosclerosis Society recommends this simple diagnostic path:- Stop the statin immediately if muscle pain starts
- Check CK levels
- If pain continues after 3 months, test for anti-HMGCR antibodies
- If positive, refer to a neuromuscular specialist
Too many patients are left waiting, thinking it’ll pass. But with SAAM, every month without treatment makes recovery harder.
What Actually Works to Fix It
For simple myalgia, stopping the statin usually fixes things in 1-2 weeks. But for myositis and especially SAAM, it’s not that simple.- CoQ10 supplements? Some people swear by them. But studies are mixed. Only 3 out of 7 trials showed real improvement. Don’t rely on it alone.
- Immunosuppressants? This is the gold standard for SAAM. Prednisone (1 mg/kg/day) plus methotrexate or mycophenolate helps 60-70% of patients recover within a year. Delay treatment beyond 12 months? Your chance of full recovery drops from 65% to 28%.
- IVIG therapy? Used in severe, stubborn cases. One study showed 75% response with ravulizumab, a newer complement inhibitor still being tested.
- Statin rotation? If you had a bad reaction to simvastatin, try rosuvastatin. One 2021 study found 73% of patients tolerated the switch.
- Intermittent dosing? Taking atorvastatin every other day cut muscle pain in half for 40% of patients in the IMPROVE-IT trial.
There’s no one-size-fits-all fix. But the key is early action. Don’t wait for your doctor to suggest a biopsy or antibody test. If your pain doesn’t vanish after a couple of weeks off statins, ask for it.
What You Can Do Right Now
If you’re on a statin and feel muscle pain:- Don’t ignore it. Write down when it started, where it hurts, and how bad it is.
- Get a CK blood test-even if your doctor says it’s “probably just soreness.”
- Check your vitamin D and thyroid levels. Low levels make muscle pain worse.
- Ask about drug interactions. Are you on amiodarone? A fibrate? A strong antibiotic? These can turn a safe statin dose into a dangerous one.
- If pain lasts longer than 2 weeks after stopping the statin, demand an anti-HMGCR antibody test.
And if you’ve been told it’s “just aging” or “fibromyalgia” but your symptoms are getting worse? Get a second opinion. See a neurologist or rheumatologist who specializes in muscle disease. You’re not imagining it.
The Bigger Picture
Statin myopathy isn’t just a side effect-it’s a systemic failure in how we manage chronic disease. We prescribe statins like they’re vitamins. But they’re powerful drugs with real, sometimes irreversible, consequences. The FDA recorded over 21,000 statin-related muscle injury cases between 2010 and 2020. Atorvastatin (Lipitor) made up 43% of those reports-even though it’s only prescribed 28% of the time. That tells you something: it’s not just about dose. It’s about who you are, your genes, and how your body reacts. The future is personalization. By 2030, doctors may use genetic tests to pick the right statin for you before you even start-cutting muscle pain risk by 30-40%. But until then, you have to be your own advocate.Statin therapy saves lives. But it shouldn’t cost you your mobility, your strength, or your quality of life. If your muscles are paying the price, it’s time to ask: is there a better way?
Can statin muscle pain go away on its own?
Yes-but only if it’s simple myalgia. For most people, muscle pain from statins fades within 1-2 weeks after stopping the drug. But if the pain persists beyond two weeks, or gets worse after stopping, it could be myositis or immune-mediated myopathy. These don’t resolve on their own and require medical intervention.
Is CoQ10 supplementation effective for statin muscle pain?
Some people report feeling better taking CoQ10, but the science is inconsistent. Out of seven randomized trials, only three showed significant improvement. It’s not a guaranteed fix, and it shouldn’t replace stopping the statin or seeking medical advice if symptoms are severe.
Can I switch to a different statin if I have muscle pain?
Yes, many people can tolerate a switch. For example, if simvastatin caused pain, switching to rosuvastatin or pravastatin often works. One study found 73% of patients who couldn’t tolerate simvastatin handled rosuvastatin well. But this doesn’t work for everyone, especially those with immune-mediated myopathy.
How do I know if I have immune-mediated myopathy?
Look for these signs: progressive weakness in shoulders and hips, CK levels above 2,000 IU/L, symptoms that get worse after stopping the statin, and no improvement after 3 months. A blood test for anti-HMGCR antibodies confirms it. A muscle biopsy showing necrotic fibers with little inflammation is the gold standard.
What happens if I ignore statin muscle pain?
Ignoring it can lead to permanent muscle damage, especially in immune-mediated cases. Delayed treatment means lower chances of recovery. Patients treated within six months of symptoms have a 65% chance of full remission. Those who wait over a year? Only 28% recover fully. Plus, continuing statins can trigger rhabdomyolysis-a life-threatening condition that can cause kidney failure.
Are there alternatives to statins for lowering cholesterol?
Yes. Ezetimibe, PCSK9 inhibitors (like evolocumab), and bempedoic acid are non-statin options that lower LDL without the same muscle risks. Lifestyle changes-diet, exercise, weight loss-also help. But for high-risk patients, statins remain the most effective. The goal is to find a safe version, not to stop treatment entirely.
Next Steps: What to Do If You’re Affected
If you’re experiencing muscle pain on a statin:- Stop the statin and call your doctor. Don’t wait.
- Request a CK test and thyroid/vitamin D panel.
- If pain lasts more than 14 days, ask for anti-HMGCR antibody testing.
- If diagnosed with immune-mediated myopathy, see a neuromuscular specialist immediately.
- Don’t assume you can’t take statins again-some people successfully restart with lower doses or different types.
- Track your symptoms. Keep a log of pain, weakness, and fatigue. It helps your doctor spot patterns.
Your heart health matters. But so does your ability to walk, climb stairs, or lift your grandchild. You don’t have to choose between them. With the right information and action, you can protect both.

Chloe Hadland
January 24, 2026 AT 03:06Been on atorvastatin for 3 years and started getting this weird leg cramp at night. Thought it was just aging until I read this. Stopped it cold turkey and within 10 days the cramps vanished. My doctor shrugged like it was normal. Turns out it wasn't. Thanks for laying this out so clearly
Juan Reibelo
January 25, 2026 AT 21:45Finally! Someone who gets it. I was told for 14 months that I had 'fibro'-until my CK hit 3,200. Anti-HMGCR positive. IVIG saved me. But I had to beg, scream, and bring printouts to three different doctors before anyone listened. Don’t let them gaslight you. Muscle pain isn’t 'just stress.' It’s biology.
Michael Camilleri
January 27, 2026 AT 19:07Look I get it people are scared of statins but let’s be real here-most of you are just mad you have to take a pill for your own bad choices. Eat better. Move more. Stop blaming Big Pharma for your sedentary lifestyle. Statins save lives. If your legs hurt maybe you should’ve eaten less bacon
Marlon Mentolaroc
January 28, 2026 AT 03:15Interesting breakdown but here’s the real data: 87% of statin myopathy cases occur in patients over 65 on high-dose statins + amiodarone. That’s not random-it’s a pharmacokinetic bomb. Also CoQ10? Useless unless you’re taking 200mg+ daily and even then, only helps myalgia. For SAAM? Only immunosuppression works. Period.
Don Foster
January 29, 2026 AT 16:55Anyone else notice how the FDA’s database shows Lipitor accounts for nearly half of all statin muscle injury reports? That’s not coincidence. It’s because it’s the most prescribed and the most potent. And yet doctors still push it like it’s aspirin. We need mandatory genetic screening before prescribing. Not optional. Mandatory. My SLCO1B1 variant cost me six months of mobility
Phil Maxwell
January 31, 2026 AT 08:24I switched from simvastatin to pravastatin after 6 weeks of soreness. No more pain. My CK dropped to normal. My doc didn’t even mention the switch option. Just said 'try again next month.' Glad I did my own research. Maybe more docs should read Reddit too
Karen Conlin
January 31, 2026 AT 08:41My mom had SAAM. Took her 18 months to get diagnosed. She’s 72. Now she’s on monthly IVIG and can walk again. But she almost lost her independence. Please-if you’re hurting, don’t wait. Don’t accept 'it’s just aging.' Get the antibody test. Advocate for yourself. You’re not being dramatic. You’re being smart. And if your doctor won’t listen? Find another one. Your muscles matter more than their schedule
Tommy Sandri
February 1, 2026 AT 10:15As a physician in the UK, I’ve seen this pattern repeatedly. The diagnostic delay is tragic. We need better education for GPs. The EAS guidelines are clear-but rarely followed. The solution isn’t to stop statins. It’s to personalize them. Genetic testing, baseline CK, and early antibody screening should be standard for patients over 50 on high-dose regimens. This isn’t alarmism-it’s clinical best practice
asa MNG
February 3, 2026 AT 04:08OMG I THOUGHT I WAS GOING CRAZY!! I was on rosuvastatin and started feeling like my arms were made of lead… then I couldn’t lift my coffee mug. My doc said ‘you’re just tired’ 😭 I stopped it and 3 weeks later I could lift weights again. CoQ10 helped a little but the real fix was just STOPPING. pls trust your body. dont listen to the dr who says ‘its all in your head’ 🤕💪