SAH Symptom Checker
This tool helps you assess whether your symptoms might indicate a subarachnoid hemorrhage (SAH). If you experience sudden severe headache or other warning signs, seek emergency medical care immediately.
Select all symptoms you are experiencing:
Subarachnoid hemorrhage sounds like medical jargon, but it’s a life‑threatening bleed that can strike without warning. If you or a loved one ever feel a sudden "worst‑ever" headache, you need to recognize why that could be a sign of something far more serious than a migraine.
TL;DR - Quick Takeaways
- SAH is bleeding into the space surrounding the brain, often from a ruptured aneurysm.
- Key symptom: "thunderclap" headache that peaks within seconds.
- Immediate CT scan is the gold‑standard test; if negative, a lumbar puncture may still be needed.
- Treatment usually involves surgical clipping or endovascular coiling, followed by intensive monitoring.
- Control blood pressure, quit smoking, and manage cholesterol to lower future risk.
What Exactly Is a Subarachnoid Hemorrhage?
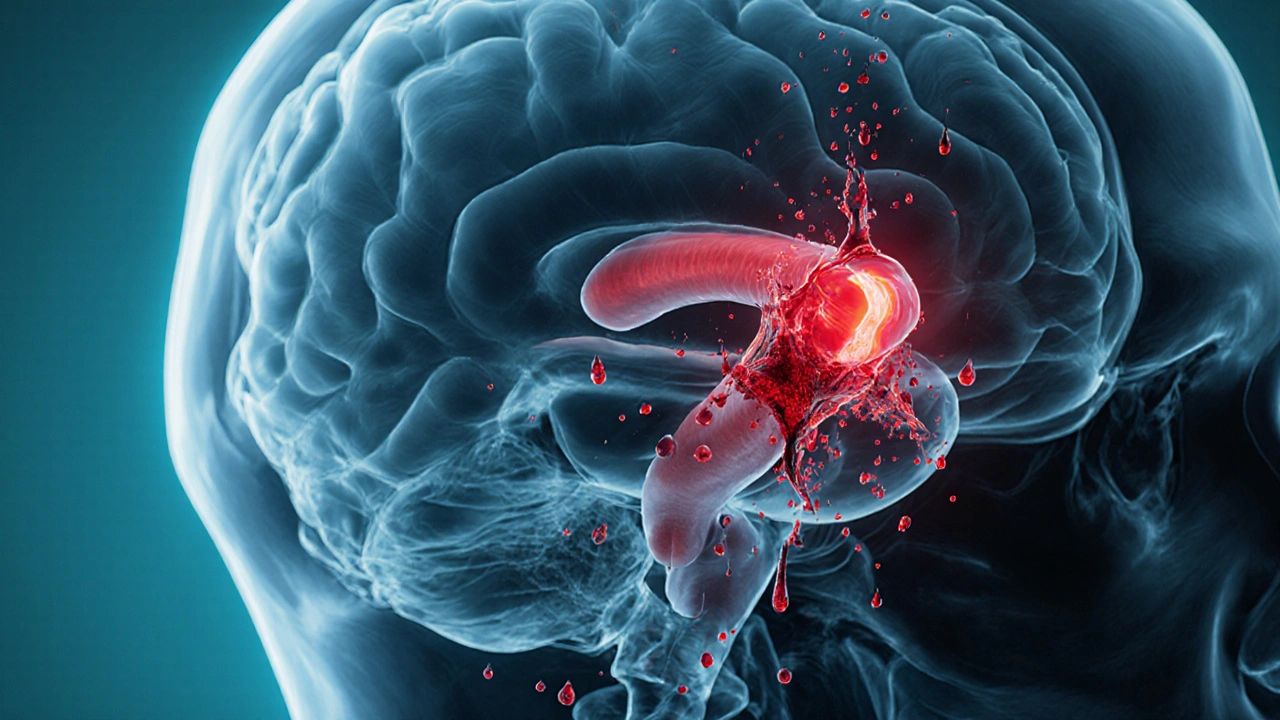
When a blood vessel ruptures in the subarachnoid space-the thin fluid‑filled layer between the brain and its outer covering-blood spills directly onto the brain surface. This sudden surge of blood raises intracranial pressure, irritates the lining (the meninges), and can quickly shut down vital brain functions.
According to the World Health Organization, SAH accounts for roughly 5% of all strokes but carries a mortality rate of 30%-40% within the first month.
Subarachnoid hemorrhage is a type of stroke caused by bleeding into the subarachnoid space surrounding the brain often follows the rupture of a brain aneurysm, a weak balloon‑like bulge in a cerebral artery wall.
Causes & Major Risk Factors
While the majority of SAH cases stem from a ruptured aneurysm (about 85%), other culprits include arteriovenous malformations (AVMs), head trauma, and rare clotting disorders.
- High blood pressure: Chronic hypertension stresses arterial walls, making them prone to bulging.
- Smoking: Nicotine damages the inner lining of arteries and accelerates aneurysm growth.
- Family history: A first‑degree relative with an aneurysm raises your personal risk.
- Age & gender: Most cases occur between ages 40‑60, with women slightly more affected.
- Excessive alcohol: Binge drinking can cause sudden spikes in blood pressure, triggering rupture.
Understanding these factors helps you and your doctor decide whether screening imaging is worthwhile, especially if you have a strong family history.
Warning Signs - What Does a “Thunderclap” Headache Look Like?
The classic description is a sudden, excruciating headache that reaches maximum intensity in less than a minute. People often compare it to being struck by a bolt of lightning.
Other red‑flag symptoms include:
- Nausea or vomiting (often without a known cause)
- Stiff neck or neck pain due to meningeal irritation
- Blurred vision or double vision
- Loss of consciousness or brief fainting spells
- Seizures, especially in younger patients
If any of these appear together, call emergency services immediately. Time lost is brain lost.
How Doctors Diagnose SAH
Speed is essential. The first imaging step is a non‑contrast CT scan, which detects blood in the subarachnoid space with over 95% sensitivity within the first six hours.
When the CT scan is negative but suspicion remains high, a lumbar puncture (LP) is performed to look for xanthochromia-a yellowish discoloration of the cerebrospinal fluid that indicates older blood.
Once bleeding is confirmed, a CT angiography (CTA) or digital subtraction angiography (DSA) maps the exact location of the aneurysm, guiding treatment decisions.

Treatment Options - From the OR to the ICU
Two main strategies aim to stop the bleed and prevent re‑rupture:
- Microsurgical clipping: A neurosurgeon places a tiny metal clip at the aneurysm neck, sealing it off. This requires a craniotomy but offers a permanent solution.
- Endovascular coiling: Through a catheter inserted via the femoral artery, soft platinum coils are packed into the aneurysm, promoting clot formation. This minimally invasive approach is often preferred for deep‑lying or irregularly shaped aneurysms.
Both procedures are typically performed within 24-72 hours of diagnosis, provided the patient is medically stable.
Post‑procedure, patients are transferred to a intensive care unit (ICU) where blood pressure, oxygen levels, and neurological status are closely monitored. Managing vasospasm-a delayed narrowing of brain arteries-is a key concern during the first two weeks.
Grading the Severity - Hunt & Hess & Fisher Scores
Doctors use two scales to predict outcomes:
- Hunt and Hess scale assesses clinical condition from grade I (mild) to grade V (coma).
- Fisher grade rates the amount of blood seen on CT, from grade 0 (no blood) to grade 4 (intracerebral or intraventricular hemorrhage).
Higher grades correlate with increased risk of vasospasm, re‑bleeding, and poorer long‑term neurologic recovery.
Recovery, Rehabilitation, and Long‑Term Outlook
Survivors face a range of challenges, from subtle cognitive deficits to severe motor impairment. Early physical, occupational, and speech therapy can dramatically improve independence.
Key statistics:
- ~50% of patients regain the ability to live independently after intensive rehab.
- ~20% experience permanent cognitive or speech problems.
- Re‑bleeding risk drops dramatically after the first two weeks if the aneurysm is secured.
Regular follow‑up imaging (usually CTA at 6 months) confirms that the clip or coil remains intact.
Preventing a Future SAH
While you can’t change your genetics, lifestyle tweaks lower the odds of aneurysm formation and rupture:
- Maintain blood pressure below 130/80mmHg; use prescribed meds consistently.
- Quit smoking - nicotine replacement or counseling can double your success rate.
- Limit alcohol to less than two drinks per day.
- Adopt a heart‑healthy diet rich in fruits, vegetables, whole grains, and omega‑3 fatty acids.
- Stay active - at least 150minutes of moderate exercise weekly reduces vascular stress.
If you have a known aneurysm that’s too small for immediate repair, your doctor may recommend periodic imaging to watch for growth.
When to Call Emergency Services
Never try to “wait it out.” Call 999 (or your local emergency number) if you notice any of the following:
- A sudden, severe headache that feels unlike anything you’ve had before.
- Neck stiffness, vision changes, or loss of consciousness.
- Vomiting without a clear gastrointestinal cause.
- Seizure activity or sudden weakness on one side of the body.
Inform the dispatcher that you suspect a possible stroke; they’ll prioritize rapid transport to a neuro‑critical care center.
| Feature | Subarachnoid Hemorrhage (SAH) | Ischemic Stroke | Intracerebral Hemorrhage |
|---|---|---|---|
| Cause | Bleeding into subarachnoid space (often aneurysm) | Blocked artery (clot) | Bleeding within brain tissue |
| Onset of headache | Thunderclap, max in seconds | Usually absent or mild | Gradual, may be severe |
| Initial CT sensitivity (first 6hr) | ~95% | ~70% | ~80% |
| Mortality (30‑day) | 30‑40% | ~10% | ~40% |
| Typical treatment | Clip or coil aneurysm, ICU care | Clot‑busting drugs, thrombectomy | Surgical evacuation, blood pressure control |
Frequently Asked Questions
What is the difference between a subarachnoid hemorrhage and a brain aneurysm?
A brain aneurysm is a weakened, bulging spot on an artery wall. When that spot bursts, blood spills into the subarachnoid space, creating a subarachnoid hemorrhage. Not every aneurysm ruptures, but a rupture always results in SAH.
Can a subarachnoid hemorrhage be prevented?
You can’t change genetics, but managing blood pressure, quitting smoking, limiting alcohol, and following a heart‑healthy diet dramatically cut the risk of aneurysm formation and rupture.
How soon after a ruptured aneurysm should surgery be performed?
Ideally within 24‑72hours, assuming the patient’s vital signs are stable. Early securing of the aneurysm reduces the chance of re‑bleeding and improves survival.
What are the long‑term cognitive effects after surviving SAH?
Around 20% of survivors experience lasting memory, attention, or executive‑function deficits. Early neuro‑rehabilitation and cognitive therapy can help mitigate these issues.
Is there a screening test for hidden aneurysms?
Magnetic resonance angiography (MRA) or CT angiography can detect unruptured aneurysms, especially in people with a family history or known risk factors. Your doctor can advise if screening is right for you.
Liam Warren
September 29, 2025 AT 02:56Great rundown, the way you broke down the pathophysiology of SAH-especially the cascade of intracranial pressure spikes-is spot on. The thunderclap headache description aligns perfectly with the classic neuro‑vascular jargon we hear in the ER. For anyone on the frontlines, that CT‑within‑6‑hours tip is pure gold. Keep the high‑impact language coming; it helps us translate complex concepts to patients in a flash.
Brian Koehler
October 2, 2025 AT 00:25Your article presents an exemplary synthesis of the current evidence, and I commend the meticulous inclusion of epidemiological data; the mortality statistics, notably the 30‑40 % figure, underscore the urgency of rapid intervention. Moreover, the distinction between clipping and coiling is articulated with commendable clarity, facilitating informed decision‑making. The preventative recommendations-blood pressure control, smoking cessation, dietary adjustments-are pragmatically sequenced, which is particularly beneficial for primary‑care clinicians. I appreciate the balanced tone, and the structured headings render navigation effortless; overall, an outstanding educational resource.
Dominique Lemieux
October 4, 2025 AT 21:53While the piece admirably attempts to condense a labyrinthine subject into digestible sections, it inadvertently glosses over several critical nuances that merit deeper scrutiny. The author’s brief mention of vasospasm, for instance, fails to convey the complex cascade of endothelin‑mediated arterial constriction that can persist for weeks. One might argue that the discussion of post‑hemorrhagic hydrocephalus is cursory at best, ignoring the fact that up to 30 % of survivors require ventriculoperitoneal shunting. The treatment timeline, presented as a tidy 24‑72‑hour window, does not account for the real‑world delays caused by anticoagulation status or comorbid cardiac instability. Moreover, the claim that smoking cessation alone reduces risk is an oversimplification; genetic predisposition and connective‑tissue disorders also play pivotal roles. The section on imaging, though thorough regarding CT sensitivity, omits the evolving role of susceptibility‑weighted MRI in detecting sub‑millimetric bleeds. A more nuanced exploration of endovascular techniques would have distinguished the subtle differences between flow‑diverting stents and traditional coil embolization. The author’s tone, while encouraging, sometimes veers into alarmist hyperbole, especially when describing the "worst‑ever" headache without contextualizing its prevalence. The rehabilitation paragraph, merely a bullet point, neglects the interdisciplinary approach involving neuro‑psychology, speech therapy, and vocational counseling. Finally, the absence of a patient‑focused narrative-stories of survivors navigating long‑term cognitive deficits-leaves a gap that could have humanized the otherwise sterile data. In sum, the article offers a solid scaffold but requires substantial elaboration to serve as a definitive guide for clinicians and patients alike.
Laura MacEachern
October 7, 2025 AT 19:21This guide does a wonderful job of demystifying a frightening condition; the clear bullet points make the warning signs instantly recognizable. I especially appreciate the emphasis on lifestyle modifications, which empowers readers to take proactive steps. The inclusion of screening recommendations for high‑risk families adds a valuable preventive angle. Overall, a compassionate and thorough resource that will undoubtedly save lives.
BJ Anderson
October 10, 2025 AT 16:50Reading this feels like a crash course in alarmist hype; the thunderclap metaphor is wielded like a siren, yet the article skirts around the gritty reality of long‑term disability that many survivors endure. It’s as if the author wants us to sprint to the ER without pausing to consider the grueling rehabilitation that follows. The surgical options are presented as a neat binary, ignoring the messy gray zones where patient comorbidities dictate compromise. Such dramatic flair may galvanize action, but it also risks sensationalizing a complex medical emergency.
Alexander Rodriguez
October 13, 2025 AT 14:18The facts are clear: a sudden, severe headache plus any additional symptom equals immediate ER. No amount of home remedies will change the outcome once the bleed starts. CT scans within six hours catch most cases, and clipping or coiling stops re‑bleeding. Knowing this saves time and lives.
Abhinav Sharma
October 16, 2025 AT 11:47Contemplating the fleeting nature of consciousness during a hemorrhage reminds us how fragile our neural tapestry truly is 🌌. The rapid cascade-from aneurysm rupture to intracranial pressure surge-mirrors the sudden bursts of insight we chase in philosophy. Yet, unlike abstract thought, this physiological storm demands urgent, concrete action 🚑. The article’s step‑by‑step guidance serves as a modern mantra: recognize, react, and restore. May we all internalize this protocol, for the sake of our loved ones and our own fleeting moments of clarity.
Welcher Saltsman
October 19, 2025 AT 09:15Hey folks, love the straightforward vibe here-no fluff, just the essentials. If you ever feel that ‘worst headache ever’, don’t wait, roll to the nearest ER. The quick CT tip is gold, and the lifestyle checklist is something we can all get behind. Thanks for keeping it real and easy to digest!
april wang
October 22, 2025 AT 06:44The comprehensive nature of this post offers a rare convergence of clinical detail and patient‑focused advice, which is indispensable for both healthcare professionals and lay readers alike. Beginning with a precise definition of subarachnoid hemorrhage, the author delineates the pathophysiological cascade in a manner that respects the reader’s intelligence while avoiding unnecessary jargon. The symptom checklist, highlighted by the ominous ‘thunderclap’ descriptor, serves as an invaluable triage tool, especially when coupled with the clear directive to seek emergency care without hesitation. Moreover, the discussion of diagnostic modalities-non‑contrast CT followed by lumbar puncture and CTA-provides a stepwise algorithm that mirrors real‑world emergency department protocols. The therapeutic section thoughtfully contrasts microsurgical clipping with endovascular coiling, noting indications, timing, and potential complications such as vasospasm, thereby equipping readers with a realistic expectation of the postoperative course. Preventive strategies are not merely an afterthought; the emphasis on blood pressure management, smoking cessation, and dietary modifications underscores the role of primary prevention in reducing aneurysm formation and rupture risk. In addition, the inclusion of follow‑up imaging recommendations bridges the acute and chronic phases of care, reminding survivors of the necessity for ongoing surveillance. Finally, the empathetic tone throughout the piece, balanced with factual rigor, transforms a potentially terrifying topic into an actionable knowledge base that can empower individuals to act decisively should the dreaded ‘worst‑ever’ headache strike.
Christopher Munt
October 25, 2025 AT 04:12That dramatic take really hits home 😔. It’s true, the aftermath can be brutal, and we need to remember the rehab battle.
Mike Creighton
October 28, 2025 AT 00:40Your critique spirals into a labyrinth of semantics, yet the underlying truth remains: the human brain, when breached, confronts mortality with a stark, indifferent elegance. In that breach, philosophy meets medicine, and the silence that follows is louder than any thunderclap.
Sarah Posh
October 30, 2025 AT 22:09Your encouragement shines through, and I’m grateful for the gentle reminder that lifestyle tweaks can make a tangible difference in outcomes.
James Knight
November 2, 2025 AT 19:37Nice flow, but you sound like a textbook robot. Real doctors don’t need that fluff.
Robert Brown
November 5, 2025 AT 17:06Your post is way too wordy.
Erin Smith
November 8, 2025 AT 14:34Totally agree its straight to the point and easy to read
George Kent
November 11, 2025 AT 12:02Well done on the jargon, but you could have cut the fluff-serious info needs brevity!!!
Jonathan Martens
November 14, 2025 AT 09:31Sure, philosophy about brain bleeds is exactly what the ER needs, keep the emojis coming
Kendra Barnett
November 17, 2025 AT 06:59You nailed the essentials, thanks for keeping it clear and to the point.
Warren Nelson
November 20, 2025 AT 04:28I hear you, man. That short burst of empathy is exactly what we need after a dramatic description. It reminds us that behind the clinical facts there are real people coping with fear and recovery.
Jennifer Romand
November 23, 2025 AT 01:56One must commend the delicate balance of optimism and clinical realism you have achieved; it elevates the discourse beyond mere informational exchange.