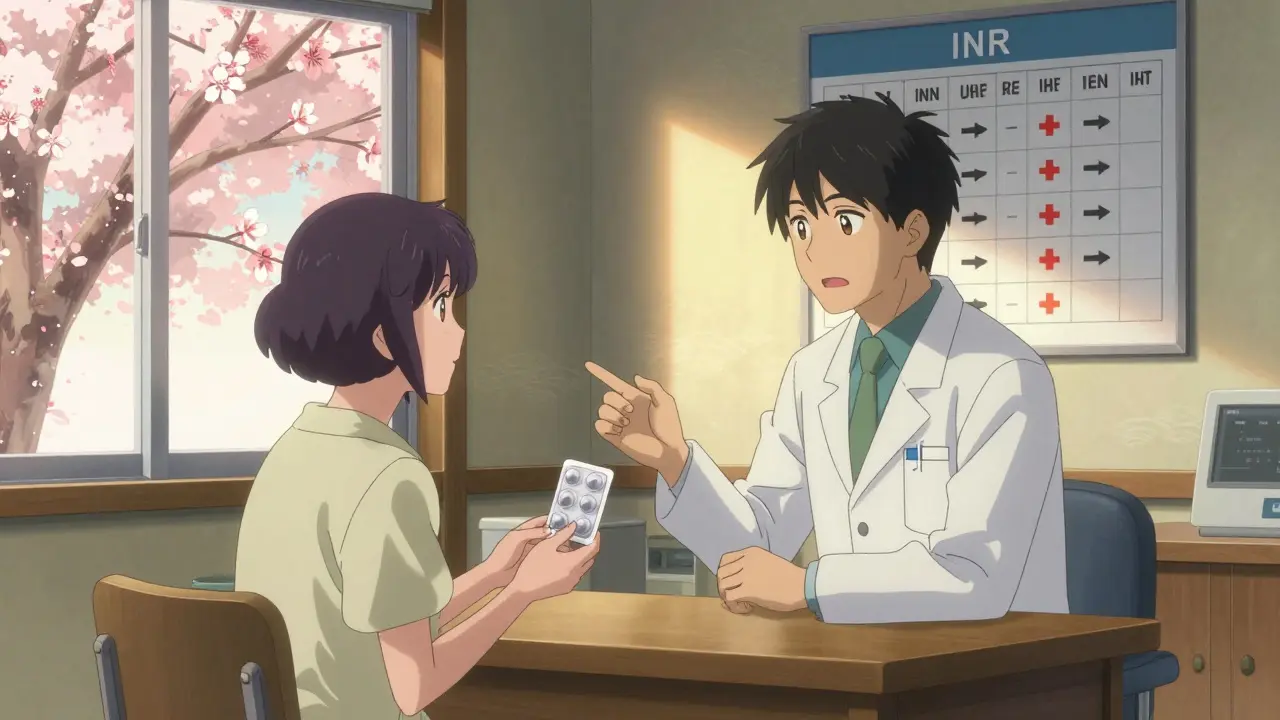
DOAC Switching Safety Calculator
Check Your Switching Safety
This tool helps determine if it's safe to switch from warfarin to a DOAC based on your INR level and kidney function. Always consult your healthcare provider before making changes to your anticoagulation therapy.
Switching from warfarin to a direct oral anticoagulant (DOAC) can simplify your life-but only if it’s done right. Thousands of people in the UK and beyond make this change every year to avoid frequent blood tests, reduce dietary restrictions, and lower the risk of serious bleeding. But this isn’t a simple swap. Get it wrong, and you could face a stroke, a dangerous bleed, or both. There’s no room for guesswork.
Why switch from warfarin at all?
Warfarin has been the go-to blood thinner for over 70 years. But it’s finicky. You need regular INR tests-sometimes every week-to make sure your blood isn’t too thin or too thick. That means more clinic visits, more finger pricks, and constant worry about what you eat. Broccoli, kale, spinach? Suddenly, your salad isn’t so simple. DOACs like dabigatran, rivaroxaban, apixaban, and edoxaban changed that. They work more predictably. No weekly blood tests. Fewer food interactions. And for most people, a lower risk of brain bleeds. The RE-LY trial showed intracranial hemorrhage rates dropped from 4.0 to 2.7 per 100 patient-years when switching from warfarin to dabigatran. But here’s the catch: DOACs aren’t magic. They still carry risks. And switching between them? That’s where things get tricky.When is switching NOT safe?
Not everyone can switch. Some people absolutely should stay on warfarin. If you have a mechanical heart valve, DOACs are off the table. Studies show they don’t protect these valves well enough. The risk of clotting is too high. This isn’t a debate-it’s a firm guideline from the Scottish Community Pharmacy and the European Society of Cardiology. You also shouldn’t switch if you have:- Severe kidney disease (CrCl under 15-30 mL/min, depending on the DOAC)
- Advanced liver disease (Child-Pugh Class C)
- Are pregnant or breastfeeding
How to switch safely: The INR rules
The single biggest mistake people make? Starting the DOAC too soon after stopping warfarin. Warfarin sticks around in your system for days. Its half-life is 36 to 48 hours. If you start a DOAC while warfarin is still active, your blood can become dangerously thin. Too late, and you risk a clot. Here’s what the guidelines say, based on INR levels:- INR ≤ 2.0: Start the DOAC immediately.
- INR 2.0-2.5: Start the DOAC immediately-or wait until the next day.
- INR 2.5-3.0: Wait 1-3 days. Recheck your INR.
- INR ≥ 3.0: Delay the switch. Recheck in 3-5 days.
What about bleeding risks during the switch?
Yes, DOACs cause less brain bleeding than warfarin. But during the transition, you’re vulnerable. The period when you stop one drug and start another is a tightrope walk. Your blood’s anticoagulant effect can dip too low-or spike too high. Some patients report increased stomach bleeding right after switching. Why? Because both drugs are active at the same time if timing is off. The American Heart Association warns: “INRs can be falsely elevated by DOACs.” That means if you get a blood test too soon after starting your DOAC, your INR might look high-even though it’s not measuring warfarin anymore. Your doctor needs to know this to avoid misreading results. Also, DOACs wear off fast. Their effect drops by 50% in 12-24 hours after your last dose. That’s why missing a pill is more dangerous than with warfarin. If you skip one dose of apixaban, your protection drops fast. No safety net.
Dabigatran has special rules
If you’re switching to dabigatran, there’s one thing no one talks about enough: storage. Dabigatran is moisture-sensitive. If you put it in a dosette box or pill organizer, humidity can ruin it. It might not work. The Royal Pharmaceutical Society is clear: “Keep dabigatran in its original blister pack.” All other DOACs can go in organizers-but not this one. Also, if you’re having surgery, timing matters even more. For someone with normal kidney function (CrCl 90 mL/min), dabigatran should be held 24-36 hours before a low-risk procedure. But if your kidneys are weaker (CrCl 45 mL/min) and you’re having major surgery? Hold it for 96-108 hours. That’s four full days. Your surgeon and pharmacist need to be on the same page.What about kidney and liver checks?
You don’t need weekly INRs anymore. But you still need blood tests. Your kidneys handle most DOACs. If they start to slow down, the drug builds up. That means more bleeding risk. Experts recommend checking kidney function every 6-12 months if you’re stable. More often if you’re older, have diabetes, or high blood pressure. Liver health matters too. Severe liver disease can mess with how your body processes DOACs. If you have cirrhosis or high liver enzymes, your doctor needs to weigh the risks carefully.What if you miss a dose?
This is where DOACs feel less forgiving than warfarin. If you miss a dose of apixaban or rivaroxaban, take it as soon as you remember-if it’s within 12 hours. If it’s more than 12 hours, skip it. Don’t double up. For dabigatran, the window is 6 hours. After that, skip it. For edoxaban, it’s 12 hours. Doubling up can push your blood too thin. Missing a dose can leave you unprotected. That’s why setting phone alarms or using a pill box (except for dabigatran) is critical.Reversing DOACs: What happens if you bleed?
Warfarin can be reversed quickly with vitamin K or fresh plasma. DOACs? Not so easy. There are specific reversal agents-but they’re expensive and not always available.- Idarucizumab reverses dabigatran.
- Andexanet alfa reverses rivaroxaban, apixaban, and edoxaban.
What about cost?
In the UK, NHS prescriptions are capped at £9.95 per item, regardless of the drug. So cost isn’t a barrier here. But in other countries-like the US-DOACs can cost $500-$700 a month. Warfarin? $10-$30. That’s a huge difference. If you’re paying out of pocket, this matters. But in the UK, it shouldn’t influence your decision.What you must do before switching
Don’t just show up at your GP and ask to switch. Do this first:- Check your latest blood results: INR, kidney function (eGFR or CrCl), liver enzymes, and full blood count-all within the last 6 months.
- Calculate your creatinine clearance using the Cockcroft-Gault formula. Your doctor should do this, but know what it is.
- Confirm your INR is in the safe range for your chosen DOAC.
- Ask if your kidney or liver function needs retesting.
- Get written instructions on when to stop warfarin and when to start the DOAC.
- Ask for an anticoagulant patient alert card and an AF information leaflet.
- Book a follow-up with your pharmacist for the New Medicine Service.
What to watch for after switching
The first few weeks matter most. Watch for:- Unusual bruising or bleeding (nosebleeds that won’t stop, bleeding gums, blood in urine or stool)
- Severe headaches, dizziness, vision changes (possible brain bleed)
- Swelling, pain, or warmth in your leg (possible DVT)
- Chest pain or shortness of breath (possible pulmonary embolism)
Final thought: It’s a team effort
Switching from warfarin to a DOAC isn’t something you do alone. It needs your GP, your pharmacist, your cardiologist, and you. The Royal Pharmaceutical Society says it clearly: “Patients should only be switched by clinicians with experience in managing anticoagulation.” If your doctor hasn’t done this before, ask for a referral to a specialist anticoagulation clinic. This isn’t a decision to make over a 10-minute appointment. It’s a life-changing one. Do it right, and you’ll have fewer tests, fewer restrictions, and better protection. Do it wrong, and the consequences can be deadly.Can I switch from warfarin to a DOAC if I’ve had a stroke before?
Yes-but only under strict supervision. If you’ve had a recent stroke or TIA, your doctor must ensure there’s no gap in protection. Stopping warfarin too early can cause another stroke. Your INR must be checked right before switching, and the DOAC should start immediately once the INR is safe. Experts warn that skipping this step increases stroke risk significantly, especially in non-valvular atrial fibrillation.
Do I still need to avoid certain foods with DOACs?
Not like with warfarin. DOACs don’t interact with vitamin K-rich foods like spinach, broccoli, or kale. You can eat them normally. But grapefruit juice can affect rivaroxaban and apixaban slightly, so it’s best to avoid large amounts. Alcohol should also be limited-more than 2-3 units a day increases bleeding risk.
What if I need surgery or a dental procedure?
You’ll need to pause your DOAC, but not as long as with warfarin. For minor procedures like tooth extractions, you may only need to skip 1-2 doses. For major surgery, hold it for 2-5 days depending on your kidney function and the procedure’s bleeding risk. Always tell your surgeon or dentist you’re on a DOAC. Never stop without medical advice.
Can I take other medications with a DOAC?
Many can, but not all. NSAIDs like ibuprofen and naproxen increase bleeding risk. Some antibiotics (like clarithromycin) and antifungals (like fluconazole) can raise DOAC levels dangerously. Always check with your pharmacist before starting any new medicine-even over-the-counter ones. Your DOAC is not as forgiving as warfarin when it comes to drug interactions.
How often do I need blood tests after switching?
No more INR tests. But you’ll still need kidney function checks-every 6-12 months if you’re stable. If you’re over 75, have diabetes, or high blood pressure, your doctor may test every 3-6 months. Liver function tests are also recommended annually. Don’t skip these. Your DOAC dose may need adjusting.
Is one DOAC better than the others?
It depends. Apixaban has the lowest bleeding risk in studies. Dabigatran is good for stroke prevention but needs careful storage. Rivaroxaban is taken once daily, which helps with adherence. Edoxaban is often used in patients with moderate kidney issues. Your doctor picks based on your kidney function, age, weight, and other conditions-not just price or convenience.
Doreen Pachificus
January 5, 2026 AT 19:21Been on apixaban for two years now. No more weekly finger pricks. I still eat my kale salads like nothing happened. The only downside? Forgetting to take it sometimes. Set three alarms now. Works like a charm.
Also, never put it in a pill organizer. Learned that the hard way when my bottle got damp and the pills turned to mush. Don't be me.
jigisha Patel
January 7, 2026 AT 13:11While the article presents a clinically accurate overview, it lacks critical context regarding real-world adherence patterns. A 2022 JAMA study demonstrated that 38% of DOAC patients discontinue therapy within 12 months due to perceived lack of efficacy or minor bleeding events. The psychological burden of self-managing anticoagulation without INR feedback is significantly underestimated in public discourse. Clinical guidelines assume patient literacy and access to monitoring infrastructure, which are not universal.
Additionally, the assertion that cost is irrelevant in the UK ignores the hidden costs of pharmacist consultations, emergency visits for bleeding events, and missed workdays - all of which are rarely quantified in patient-facing materials.
Jason Stafford
January 8, 2026 AT 05:25They’re hiding something. DOACs were pushed by Big Pharma because they make WAY more money than warfarin. Why else would every doctor suddenly switch everyone? The reversal agents? Total scam. They cost $5,000 a dose and hospitals barely stock them. You think they care if you bleed out? No. They just want you on the expensive stuff.
I checked my INR last week after switching - it was 1.1. That’s not normal. That’s not safe. They told me it doesn’t matter anymore. Bullshit. They’re turning us into lab rats.
Justin Lowans
January 8, 2026 AT 20:09This is one of the most comprehensive and balanced guides I’ve read on anticoagulant transitions. The emphasis on renal function, storage protocols for dabigatran, and the nuanced INR thresholds reflects real clinical wisdom - not just textbook generalizations.
I’ve worked in pharmacy for 18 years, and I still see patients making the same mistakes: skipping doses because ‘it’s not warfarin,’ storing dabigatran in pill organizers, or assuming no diet restrictions means no lifestyle changes. This post should be mandatory reading for anyone considering the switch.
Michael Rudge
January 10, 2026 AT 08:38Wow. So you’re telling me that if I’m under 60kg or over 150kg, I’m basically a guinea pig? No one studied people who don’t fit the mold? How comforting. And here I thought medicine was science. Turns out it’s just a series of clinical trials on middle-aged white men with average BMI and perfect kidneys.
Thanks for the reminder that my body is an outlier. Maybe I should just stop taking anything and hope for the best.
Ethan Purser
January 12, 2026 AT 04:49I’ve been thinking about this a lot lately. The whole anticoagulant system is a metaphor for modern healthcare: we’re told we’re free, but we’re just trading one cage for another. Warfarin kept us chained to the lab. DOACs chain us to our phones, our pill organizers, our fear of missing a dose, our dread of bleeding out in the middle of the night with no reversal agent nearby.
We’re not being empowered. We’re being optimized. And someone’s making billions off our anxiety.
I used to trust my doctor. Now I just trust my instincts - and the fact that I still have two kidneys.
What if the real danger isn’t the clot or the bleed? What if it’s the illusion of control?
Cassie Tynan
January 13, 2026 AT 17:00So let me get this straight - you can eat your spinach again, but you can’t store your pill in a box? That’s like being told you can have freedom… as long as you don’t touch the blue cup.
Also, I love how they say ‘don’t double up’ like it’s common sense. But when you’re 72 and forget if you took it at 8am or 9am, you’re not thinking logically - you’re thinking ‘I don’t wanna die.’
DOACs are like a high-maintenance partner. Beautiful, efficient, but one wrong move and everything explodes.
Rory Corrigan
January 14, 2026 AT 21:16Just switched last month. Apixaban. Took me 3 weeks to stop checking my INR. Now I just look at my fingers - if they’re not turning purple, I’m probably okay. 😅
Also, I put my dabigatran in a pill organizer. I’m 70. I’m not dying because of humidity. If it stops working, I’ll know. And I’ll call my pharmacist. Done.
Charlotte N
January 15, 2026 AT 00:48my kidney function is 42 so i’m on a lower dose of edoxaban and honestly i didn’t know i needed to get it checked every 6 months i thought once was enough
also grapefruit juice is fine right i mean i drink like one glass a week and i’ve been fine so far
should i be worried
bob bob
January 15, 2026 AT 07:31I switched six months ago. I used to hate blood tests. Now I hate remembering to take my pill. But I’d take the pill any day.
Also, my pharmacist gave me a free pill box and wrote my schedule on it in marker. Best thing that’s ever happened to me.
Allen Ye
January 15, 2026 AT 23:55There’s a deeper philosophical tension here that the article barely touches - the erosion of patient agency through medicalized convenience. Warfarin forced us into a rhythm of vigilance, of bodily awareness - we were forced to monitor, to reflect, to engage with our own physiology on a weekly basis. DOACs offer freedom, yes - but at the cost of detachment. We no longer feel the weight of our condition. We don’t know our INR. We don’t track our diet. We don’t even know how our kidneys are doing until the lab report comes back with a red flag.
Is this liberation… or quiet surrender?
Consider this: when you stop measuring your blood, you stop listening to it. And when you stop listening, you stop being a participant in your own survival. You become a consumer of a system that tells you when to take a pill and when to worry.
I’m not saying go back to warfarin. I’m saying: don’t let convenience numb you. Your body isn’t a machine to be optimized - it’s a conversation. And if you stop asking questions, it’ll stop answering.
Check your eGFR. Talk to your pharmacist. Read the leaflet. Don’t just click ‘accept’ and move on. Your life isn’t a software update. It’s a lived experience. And if you treat it like one, you’ll wake up one day wondering why you feel so… empty.
And maybe that’s the real side effect they never told you about.