When someone vomits blood or passes black, tarry stools, it’s not just unpleasant-it’s a medical emergency. Upper GI bleeding can come from a simple stomach ulcer or something far more dangerous like ruptured varices in the liver. The difference between life and death often comes down to how fast you recognize it and how quickly you act.
What Exactly Is Upper GI Bleeding?
Upper gastrointestinal bleeding means blood is coming from somewhere in the upper part of your digestive tract-your esophagus, stomach, or the first part of your small intestine (duodenum). It’s not rare. About 100 out of every 100,000 adults in the U.S. experience it each year. That’s roughly 300,000 hospitalizations annually. And it’s getting more common as the population ages. People over 80 are three times more likely to bleed than those under 50.The most common cause? Peptic ulcers. They account for 40 to 50% of cases. These are open sores in the stomach or duodenum, often caused by H. pylori bacteria or long-term use of NSAIDs like ibuprofen or aspirin. The second big culprit? Esophageal varices-swollen veins in the esophagus, usually from advanced liver disease. They’re less common but far more deadly. About 1 in 5 people with variceal bleeding won’t survive the next six weeks.
Other causes include erosive gastritis, Mallory-Weiss tears (from violent vomiting), esophagitis, and even stomach cancer. And yes, even common medications like SSRIs (antidepressants) can double your risk of bleeding. It’s not just about what you eat-it’s about what you take, what you’ve had, and what’s going on inside your body.
Recognizing the Signs Before It’s Too Late
You can’t ignore these symptoms. They’re your body screaming for help.- Hematemesis: Vomiting bright red blood means active bleeding. If it looks like coffee grounds, the blood has been sitting in your stomach-still serious, but maybe a little slower.
- Melena: Black, sticky, foul-smelling stools. That’s digested blood. It doesn’t mean it’s minor-it means the bleed is upstream, likely in the stomach or duodenum.
- Hematochezia: Bright red or maroon stools. This can happen with massive bleeding, when blood rushes through too fast to be digested.
- Dizziness, fainting, rapid heartbeat: Your body is trying to compensate for lost blood. A heart rate over 100 beats per minute and systolic blood pressure below 90 mmHg are red flags.
One patient on Reddit described waking up at 3 a.m. coughing up coffee-ground material. He ended up in the ER, got three units of blood, and stayed in the hospital for eight days. Another person had black stools dismissed as “iron supplements” for two weeks-until they collapsed. Their hemoglobin was 5.8. Normal is 12 to 16. That’s life-threatening.
Don’t wait. Don’t assume it’s heartburn. Don’t think it’ll go away. If you’re vomiting blood or passing black stools, go to the ER. Now.
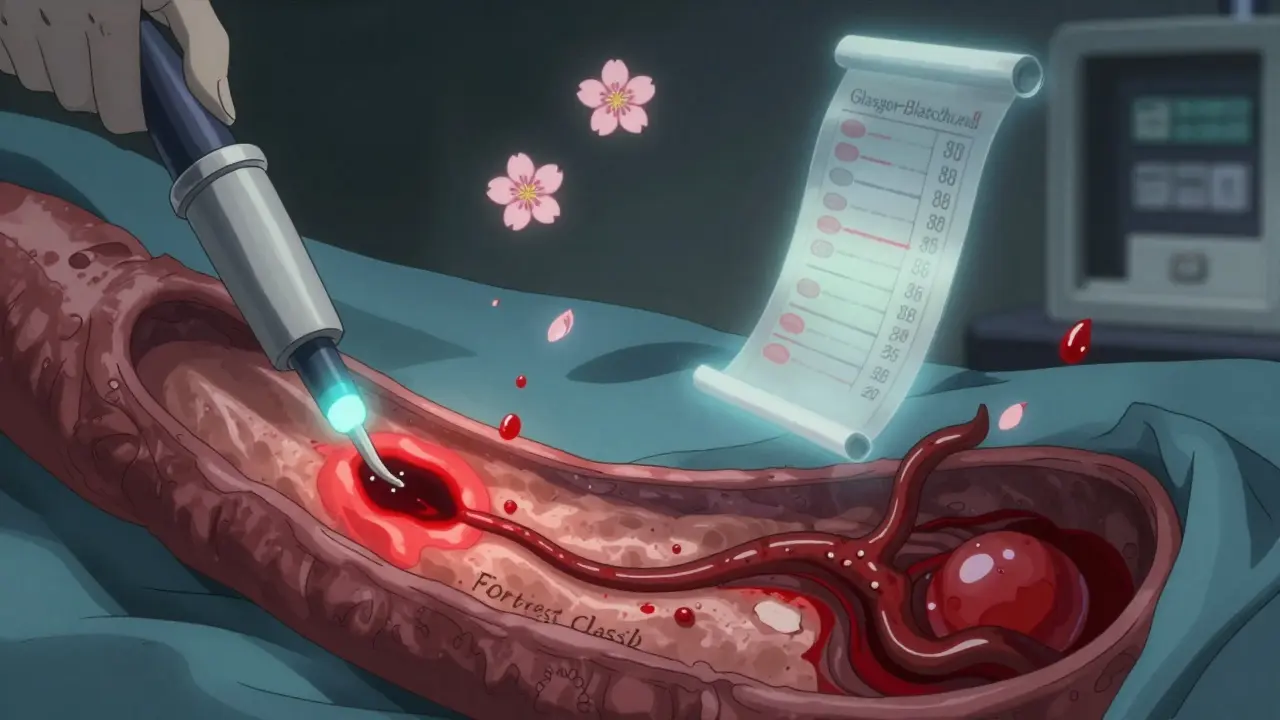
How Doctors Assess the Danger: The Glasgow-Blatchford Score
Not every case needs the same level of urgency. That’s why doctors use the Glasgow-Blatchford score. It’s not a guess. It’s based on hard numbers:- Hemoglobin level (below 12.9 g/dL for men, below 11.9 for women)
- Systolic blood pressure (below 100 mmHg)
- Pulse rate (above 100 bpm)
- Presence of melena
- History of syncope (fainting)
- Signs of liver or heart disease
A score of 2 or higher means you need hospital care. A score of 0? You might be able to go home safely. In fact, studies show that 15% of patients with upper GI bleeding can be managed without hospitalization if their score is low. That’s a game-changer.
But here’s the catch: doctors who rely only on symptoms or guesswork miss the mark. One expert said 30% of low-risk patients get unnecessary treatments because they skip the score. That’s why it’s now standard in every major hospital in the U.S. and Europe.
What Happens in the ER: Stabilization First
Before you even get an endoscopy, your body has to be stabilized. No exceptions.- IV fluids are started immediately to maintain blood pressure.
- Oxygen is given if you’re dizzy or struggling to breathe.
- Blood tests: CBC to check hemoglobin, INR to see how well your blood clots, and BUN-to-creatinine ratio. If that ratio is above 30:1, it’s 69% likely you’re bleeding from the upper GI tract.
- Transfusions? Only if your hemoglobin is below 7 g/dL or you’re symptomatic. Don’t over-transfuse. Studies show keeping hemoglobin between 7 and 9 g/dL is safer than pushing it to 10 or higher.
Each unit of packed red blood cells raises your hemoglobin by about 1 g/dL. Simple math. No guesswork.
Endoscopy: The Most Important Test
The gold standard for diagnosis and treatment? Esophagogastroduodenoscopy (EGD). This is a camera on a tube that goes down your throat to see the source of bleeding.Timing matters. The American College of Gastroenterology says: get it done within 24 hours. But the best outcomes? When it’s done within 12 hours. One study showed mortality drops by 25% when endoscopy happens early.
During the procedure, doctors use the Forrest classification to rate the bleeding risk:
- Class Ia: Spurting blood. 90% chance of rebleeding without treatment.
- Class Ib: Oozing. 50% risk.
- Class IIa: Visible vessel. Also 50% risk.
If you’re in Class I or II, they don’t just look-they treat. Right then and there.
Treatment: Ulcers vs. Varices
How you treat depends entirely on what’s bleeding.For ulcers and non-variceal bleeding:
- High-dose IV proton pump inhibitors (PPIs): 80 mg bolus, then 8 mg/hour infusion. This cuts rebleeding from 22.6% to 11.6%.
- Endoscopic therapy: Epinephrine injection to shrink blood vessels, then either heat (thermal coagulation) or clips (hemoclips) to seal the spot. Success rate? 90-95%.
For esophageal varices:
- Vasoactive drugs: Terlipressin or octreotide. These drugs shrink the veins and reduce pressure in the liver.
- Antibiotics: Ceftriaxone 1g daily. Prevents infections that can kill you when your liver is already failing.
- Band ligation: Rubber bands placed around the varices. It’s the preferred method. Reduces rebleeding from 60% to 25%.
Sclerotherapy (injections to harden veins) used to be common. Now it’s mostly replaced by banding. Why? Better results, fewer complications.

What’s New in 2026
Medicine doesn’t stand still. Two big advances are changing the game:Hemospray: This is a fine powder sprayed directly onto bleeding sites during endoscopy. It forms a physical barrier. In tough cases where clips or heat don’t work, it stops bleeding in 92% of cases.
AI-assisted endoscopy: New systems use artificial intelligence to spot tiny signs of bleeding that human eyes miss. In one trial, AI detected bleeding with 94.7% accuracy-compared to 78.3% for experienced doctors. But here’s the catch: current AI tools are less accurate in Black and Hispanic patients because the training data was mostly from white populations. That’s a problem researchers are fixing now.
The NIH is running a massive study called UGIB-360, tracking 10,000 patients to build personalized risk models using genetics, gut bacteria, and clinical history. Results are expected late 2025. This could mean your treatment is tailored to your body-not just your symptoms.
What Patients Do Afterward
Surviving the bleed is only half the battle. The other half is preventing the next one.- Stop NSAIDs. If you need pain relief, switch to acetaminophen. Always check with your doctor first.
- If you have H. pylori, you’ll get antibiotics to clear it. This cuts ulcer recurrence by 90%.
- Alcohol? Cut it out. Especially if you have liver disease.
- Antidepressants? Don’t stop them on your own. Talk to your doctor. The risk is real, but so is the risk of untreated depression.
A 2022 study found 68% of patients were anxious about bleeding again within 30 days. Over 40% changed their diet-cutting caffeine, spicy food, alcohol-without being told to. That’s good. But 31% stopped their meds without consulting anyone. That’s dangerous.
Follow-up is key. Hospitals that use a full “Upper GI Bleed Bundle”-rapid assessment, risk scoring, early PPIs, endoscopy within 12 hours, and follow-up within 72 hours-cut their 30-day death rate from 8.7% to 5.3%.
Final Reality Check
Upper GI bleeding is scary. But it’s not mysterious. It’s predictable. It’s treatable. And it’s preventable in most cases.If you’re over 65, take NSAIDs regularly, have liver disease, or have a history of ulcers-you’re at higher risk. Know the signs. Don’t wait. Don’t dismiss black stools or vomiting. Get checked.
Doctors aren’t infallible. One patient was told his black stools were from iron pills. He collapsed. His hemoglobin was 5.8. He survived. But not everyone does.
Know your numbers. Know your risks. And if something feels wrong-trust your gut. Because sometimes, your gut is trying to tell you something life-saving.
What are the most common causes of upper GI bleeding?
The top causes are peptic ulcers (40-50% of cases), esophageal varices (10-20%), erosive gastritis (15-20%), and Mallory-Weiss tears (5-10%). Less common causes include esophagitis, tumors, and hiatal hernias. H. pylori infection and NSAID use are the biggest triggers for ulcers.
Is upper GI bleeding life-threatening?
Yes, especially if bleeding is rapid or untreated. Mortality rates range from 5% to 20%, depending on the cause. Variceal bleeding has a 20% death rate within six weeks. Older adults and those with liver or heart disease are at highest risk. Early treatment cuts death risk by up to 25%.
How do I know if I need to go to the ER?
Go to the ER immediately if you vomit bright red blood, pass black tarry stools, feel dizzy or faint, have a rapid heartbeat (over 100 bpm), or your blood pressure drops below 90 mmHg. Even if symptoms seem mild at first, they can worsen quickly. Don’t wait.
Can I treat upper GI bleeding at home?
No. Upper GI bleeding requires hospital care. Even if you think it’s minor, you need diagnostics like endoscopy and blood tests. Home remedies like antacids won’t stop active bleeding. Delaying care increases the risk of death or rebleeding.
What can I do to prevent future bleeding?
Avoid NSAIDs unless prescribed. If you have H. pylori, get treated with antibiotics. Quit alcohol if you have liver disease. Don’t stop antidepressants without talking to your doctor. Follow up with a gastroenterologist after your bleed. Most rebleeds happen because the root cause wasn’t addressed.
Do I need a repeat endoscopy after the first one?
Usually not. If your first endoscopy shows low-risk stigmata (like a clean base or flat spot), repeat endoscopy adds no benefit. Studies show rebleeding rates are nearly identical (4.2% vs 4.5%) with or without a second procedure. Repeat endoscopy is only done if bleeding returns or if the first one was inconclusive.
Are there new treatments on the horizon?
Yes. Hemospray, a powder that seals bleeding sites, is already in use for tough cases. AI-powered endoscopy systems are being rolled out in major hospitals-they spot bleeding with 95% accuracy, far better than human eyes. By 2030, personalized risk models based on your genes, gut bacteria, and medical history will guide prevention and treatment.

steve rumsford
January 8, 2026 AT 02:10Man i saw a guy at the gas station puke blood last year. Thought he was gonna die right there. Didn't even call 911 till his friend dragged him to the car. Scared the crap outta me. Never ignore black stools.
Paul Mason
January 9, 2026 AT 17:59Ulcers are way more common than people think. I used to take ibuprofen for my back like it was candy. One day I woke up with coffee-ground vomit and ended up in the ER. Turns out I had a 3cm ulcer. They gave me PPIs and told me to ditch the NSAIDs. Best life advice I ever got. Seriously, if you're over 50 and on painkillers daily, get checked. It's not worth it.
Andrew N
January 11, 2026 AT 02:11The Glasgow-Blatchford score is overrated. I've seen too many patients with a score of 0 who still bled out. The real issue is that hospitals rely on algorithms instead of clinical judgment. Also, the 7-9 g/dL transfusion range? That's a guideline, not a rule. Some people need more. Especially if they're active or have cardiac issues. Don't let a spreadsheet decide your treatment.
LALITA KUDIYA
January 12, 2026 AT 04:18My uncle had varices from alcohol and liver disease. He survived because they did banding fast. But he still drinks a little. I tell him every week: stop. He says he's fine. I'm scared he'll go again. Please don't wait till it's too late. 💔
Christine Joy Chicano
January 13, 2026 AT 08:07AI-assisted endoscopy is a game-changer-but the racial bias in training data is unconscionable. We're deploying tech that misses bleeding in darker skin tones because the datasets were 80% white. This isn't just a technical flaw-it's a moral failure. The NIH’s UGIB-360 study needs to prioritize diversity from day one. Otherwise, we're automating inequality.
Adam Gainski
January 13, 2026 AT 19:14Just want to add something practical: if you're on SSRIs and notice black stools, don't panic-but don't ignore it either. Talk to your doctor. Sometimes switching to an SSRI with lower bleeding risk (like sertraline over paroxetine) helps. And if you're on blood thinners, that combo is a ticking time bomb. Always tell your GI doc about every med you take-even supplements.
Alex Danner
January 14, 2026 AT 22:14That Hemospray thing? I used it last month on a 78-year-old with a bleeding Dieulafoy lesion. Clipping failed. Thermal didn't stick. Then we sprayed it-and boom, stopped cold. 92% success rate? No joke. It's not magic, but it's the closest thing we've got when everything else fails. Big win for interventional GI.
Anastasia Novak
January 16, 2026 AT 15:48Everyone's acting like this is some groundbreaking revelation. Newsflash: we've known about H. pylori and NSAIDs for 30 years. The real story? Big Pharma pushed PPIs like candy while downplaying the long-term risks-osteoporosis, kidney damage, dementia. And now they're selling AI as the savior? Please. It's all about profit, not patients.
Emma Addison Thomas
January 17, 2026 AT 00:21As someone from the UK, I’ve seen how the NHS handles this differently. We don’t rush to endoscopy unless the score is high. Saves resources. But we also have better follow-up systems-community nurses check in at 48 hours. Maybe the US could learn from that. Not everything needs to be fast. Sometimes it needs to be steady.
Kyle King
January 18, 2026 AT 13:27They're lying about the stats. The real reason GI bleeding is rising? Fluoride in the water. It weakens the stomach lining. Also, 5G radiation messes with your gut bacteria. And don't get me started on the vaccine-induced clotting that turns into ulcers. The hospitals won't tell you this because they're paid by the pharma giants. Wake up.
Kamlesh Chauhan
January 18, 2026 AT 14:15Why do we even care about this? People just get old and bleed. It's natural. I had black poop for a week once. Ate some beets. Was fine. Stop scaring people. They just want you to go to the hospital and spend your life savings on tests nobody needs.
Poppy Newman
January 20, 2026 AT 10:03My dad had a bleed last year. They did the endoscopy at 11 hours. Found a bleeding ulcer. Used clips and PPIs. He was home in 4 days. The whole process felt so smooth. I didn’t know how much tech had improved. 🙌