Fall Risk Assessment Tool
Assess Your Fall Risk
This tool helps evaluate your fall risk based on factors related to sclerosis and aging. Results will help you understand your current risk level and identify areas for improvement.
Your Fall Risk Assessment
When we talk about Sclerosis a group of chronic diseases that cause hardening or scarring of tissues, often affecting nerves, skin, or organs, the immediate question is how it behaves as we add years to our lives. The reality is a mix of predictable changes, surprising twists, and opportunities to stay active. Below, we break down what seniors with sclerosis typically notice, how to fine‑tune treatment, and where to get help before a problem becomes urgent. Expect a plain‑talk guide that respects the day‑to‑day challenges of living with this condition.
How Aging Affects Sclerosis
Age brings natural shifts in the immune system, blood flow, and nerve repair. In younger patients, the immune response that drives Multiple Sclerosis (MS) or Systemic Sclerosis (SSc) is often aggressive, leading to relapses or rapid skin changes. As you move past 60, the immune system tends to become less reactive, which can mean fewer flare‑ups but also slower healing when damage occurs.
Vascular stiffness, a hallmark of normal aging, compounds the problem. Blood vessels that already struggle to deliver oxygen to nerves in MS become less efficient, potentially heightening fatigue. In systemic sclerosis, reduced blood flow can worsen skin tightening and digital ulcers, especially in the hands and feet.
Another key element is the decline in hormone levels-especially estrogen and testosterone-which have modest anti‑inflammatory effects. The drop can subtly increase the perception of pain and affect mood, making mental health support crucial as you age.
Typical Changes in Symptoms Over Time
- Fatigue - Becomes more pronounced. Older adults often describe it as “always tired” rather than the brief energy crashes seen in younger patients.
- Mobility - Walking speed may drop 10‑15% per decade, and balance issues increase, raising fall risk.
- Vision - Optic neuritis can still flare, but cataracts and age‑related macular degeneration add extra visual strain.
- Pain - Joint and muscle aches may merge with arthritis, making it harder to pinpoint the source.
- Cognitive changes - “Brain fog” can be amplified by sleep apnea, a common comorbidity in seniors.
While some symptoms lessen-like the frequency of relapses in MS-others, such as skin tightening in systemic sclerosis, often continue to progress, just at a slower pace.
Managing Health: Lifestyle and Therapies
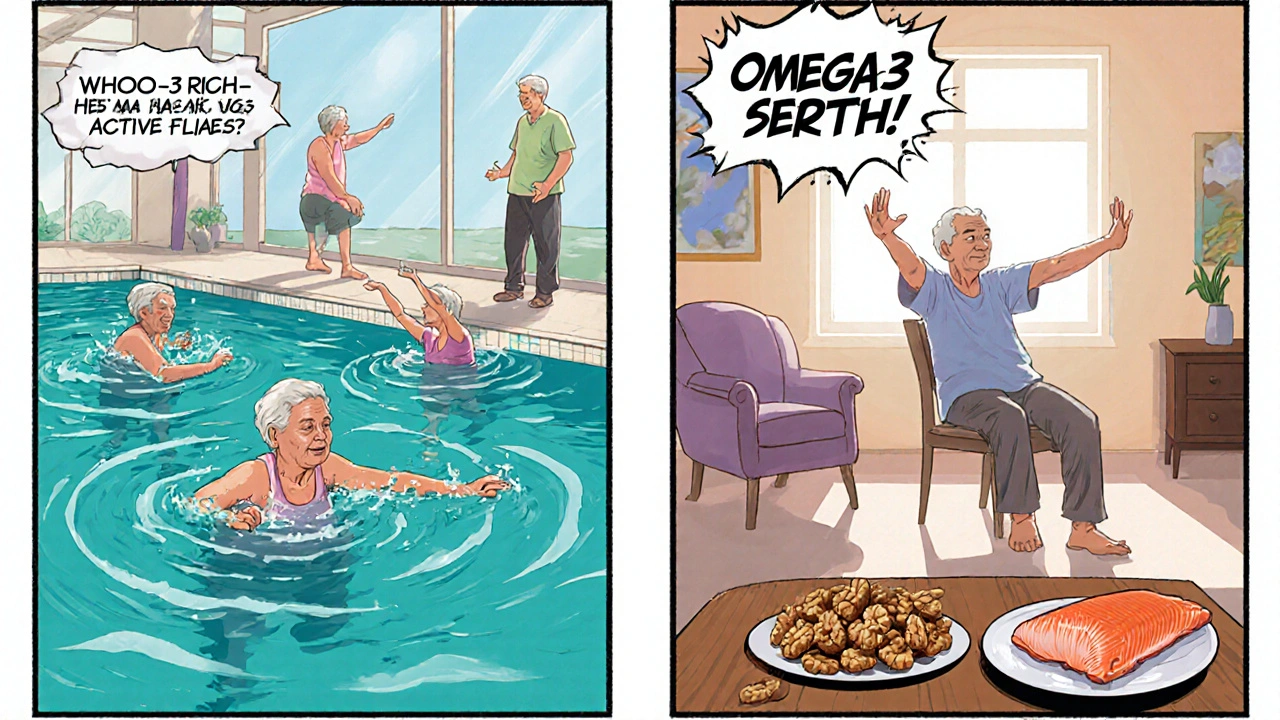
Staying active is the single most effective tool. Low‑impact cardio (walking, swimming, stationary cycling) improves circulation, reduces fatigue, and supports neuroplasticity. Pair that with Physical therapy tailored to your current strength level; a therapist can teach balance drills that cut fall risk by up to 30%.
Nutrition matters too. Diets rich in omega‑3 fatty acids-think fatty fish, walnuts, flaxseed-have modest anti‑inflammatory effects. Vitamin D levels often dip after age 50; aim for 30‑50ng/mL (checked via blood test) to support bone health and possibly modulate immune activity.
Mind‑body practices like tai chi or gentle yoga relieve stress, improve joint flexibility, and have been shown to lower perceived pain scores in sclerosis patients.
Medication Considerations for Older Adults
When you’re over 60, drug metabolism slows, and the chance of interactions climbs. Here’s a quick cheat‑sheet:
| Drug Class | Common Use | Age‑Specific Note |
|---|---|---|
| Disease‑Modifying Therapies (DMTs) | Reduce MS relapses | Monitor liver enzymes quarterly; avoid high‑dose steroids if osteoporosis present. |
| Immunosuppressants (e.g., mycophenolate) | Control systemic sclerosis | Check kidney function every 6months; watch for infections. |
| Antispasmodics | Manage muscle stiffness | Start low, increase slowly; watch for drowsiness. |
| Analgesics (acetaminophen, low‑dose NSAIDs) | Pain relief | Prefer acetaminophen; NSAIDs increase GI bleed risk with age. |
Always discuss any new over‑the‑counter supplement with your neurologist or rheumatologist; even “natural” products can interfere with blood thinners, which many seniors take for heart health.
Common Comorbidities and Their Impact
Older adults often juggle several conditions alongside sclerosis:
- Hypertension - Can worsen fatigue and increase stroke risk in MS.
- Diabetes - Slows wound healing, a concern for digital ulcers in systemic sclerosis.
- Osteoporosis - Heightens fracture risk when balance is already compromised.
- Depression - Affects medication adherence and overall quality of life.
- Sleep apnea - Exacerbates brain fog and daytime fatigue.
Addressing each comorbidity early-through blood pressure control, glucose monitoring, bone density scans, mental health counseling, and sleep studies-keeps the overall disease burden lower.
Planning for Care and Support
Think of care as a team sport. Your primary doctor, neurologist or rheumatologist, physical therapist, and a trusted family member should all be on the same page. Use a simple spreadsheet or a shared digital notebook to track medication changes, symptom logs, and upcoming appointments.
Home adaptations are often underrated. Installing grab bars, using a raised toilet seat, and ensuring good lighting can dramatically reduce falls. If skin tightening limits hand function, adaptive kitchen tools (large‑handle utensils, electric can openers) keep independence intact.
Financial planning deserves attention, too. Many insurers cover disease‑modifying therapies but may have age‑related limits. Check your Medicare Part D formulary and explore patient assistance programs offered by drug manufacturers.
When to Seek Medical Help
Red‑flag symptoms that merit immediate evaluation include:
- Sudden vision loss or double vision lasting more than 24hours.
- Rapid onset of severe weakness in one limb.
- New or worsening chest pain-could signal pulmonary hypertension in systemic sclerosis.
- Unexplained fever or chills, indicating infection.
- Significant bladder or bowel dysfunction appearing abruptly.
Call your neurologist or rheumatologist right away, or head to the emergency department if any symptom is severe or worsening fast.
Quick Reference Table: MS vs. Systemic Sclerosis in Seniors
| Feature | Multiple Sclerosis | Systemic Sclerosis |
|---|---|---|
| Primary organ affected | Central nervous system | Skin, blood vessels, internal organs |
| Typical symptom progression | Fewer relapses, more gradual disability | Skin tightening continues, organ fibrosis may appear |
| Common comorbidities | Osteoporosis, depression | Hypertension, renal involvement |
| First‑line therapy for seniors | Low‑dose interferon or glatiramer | Mycophenolate mofetil or cyclophosphamide (low dose) |
| Impact on mobility | Balance issues, spasticity | Joint contractures, Raynaud’s phenomenon |
Frequently Asked Questions
Will my sclerosis symptoms get worse after age 65?
Most people see a shift from frequent relapses to slower, steady progression. Symptoms like fatigue and balance problems often become more noticeable, but aggressive disease‑activity usually eases. Ongoing therapy and lifestyle tweaks can keep the slowdown manageable.
Can I still use disease‑modifying drugs after 70?
Yes, many seniors stay on DMTs, but dosages may be reduced and monitoring intensified. Talk with your neurologist about kidney and liver function tests before continuing.
What exercises are safest for someone with limited mobility?
Chair‑based yoga, seated tai chi, and water aerobics are excellent low‑impact options. They improve circulation without stressing joints or balance.
How do I protect my skin if I have systemic sclerosis?
Gentle moisturizers applied twice daily, protecting hands from cold, and using silicone dressings on ulcers help. Avoid harsh soaps and consider silicone gel sheets for scar management.
Is depression common in older adults with sclerosis?
Yes, rates are higher than in the general elderly population. Regular screening, counseling, and-if needed-antidepressants can improve quality of life dramatically.
Living with sclerosis and aging isn’t a one‑size‑fits‑all journey, but understanding the patterns, staying proactive with therapy, and building a solid support network can turn a potentially daunting road into a manageable, even rewarding, phase of life.

Sayam Masood
October 15, 2025 AT 17:51Time, as it stretches across the decades, gently rewires the immune orchestra, softening the once‑blaring crescendos of sclerosis. In practice, this means fewer fireworks of relapse but a slower, stubborn healing of the tissues that have been scarred.
Jason Montgomery
October 15, 2025 AT 23:25Keep moving, even if it’s just a few steps around the kitchen; those tiny bursts of activity keep the blood flowing and the mind sharp. Remember, consistency beats intensity for seniors battling sclerosis.
Jo D
October 16, 2025 AT 04:58Oh great, another “age‑related” slowdown-because apparently our bodies love to upgrade to the “turtle” firmware just when we need them to run Windows 10.
Halle Redick
October 16, 2025 AT 10:31Embracing cultural rituals-like a warm cup of ginger tea after a gentle tai chi session-can lift spirits and ease joint stiffness. Small, pleasant habits become powerful allies against the fatigue that creeps in with age.
karl lewis
October 16, 2025 AT 16:05While the guide offers a commendable overview, it occasionally wanders into generic platitudes, neglecting the nuanced pharmacokinetic shifts that seniors must navigate. A more precise discussion of renal clearance variations would have strengthened the piece. :)
Amy Martinez
October 16, 2025 AT 21:38Living with sclerosis after sixty is like learning to dance on a floor that’s slowly losing its grip.
The first step is accepting that your body’s tempo has changed, and that patience becomes a daily practice.
Fatigue, that relentless companion, may no longer be a brief dip but a steady hum that colors every activity.
Yet, research shows that regular, low‑impact movement can coax the nervous system into forging new pathways, even in older brains.
Think of a daily walk as a gentle tide, washing away stiffness while delivering fresh oxygen to compromised nerves.
Pairing that stroll with mindful breathing can calm the hormonal rollercoaster that often spikes pain perception.
Nutrition, too, plays a starring role; omega‑3 rich foods act like tiny firefighters dousing inflammatory sparks.
Don’t forget vitamin D, the unsung hero that supports both bone health and immune modulation, especially when sunlight is scarce.
For skin‑tightening concerns, silicone dressings act as soft cushions, protecting ulcers without adding extra pressure.
Simple home tweaks-like installing grab bars or using a jar opener-preserve independence that might otherwise slip away.
Mental health deserves equal focus; a weekly chat with a counselor can untangle the web of depression that often coexists with chronic illness.
If sleep apnea is a silent thief, a CPAP machine can reclaim those vital hours, sharpening cognition and easing brain fog.
Medication reviews every six months ensure that dosages remain safe as liver and kidney function evolve with age.
Trust your healthcare team, but also keep a personal log of symptoms, medications, and side effects; it becomes your advocacy handbook.
Community support groups, whether virtual or in‑person, provide a chorus of shared experiences that can lift your morale on tough days.
Ultimately, aging with sclerosis is not a sentence, but a narrative you can rewrite with resilience, knowledge, and a sprinkle of optimism.
Max Canning
October 17, 2025 AT 03:11Yo! Don't let the ‘old timer’ label hold you back-grab those water bottles and splash into a pool class. Even a 15‑minute lap can reboot your energy and give that stubborn brain fog a kick.
Nick Rogers
October 17, 2025 AT 08:45Indeed, regular exercise, balanced diet, and vigilant medication monitoring, together form a comprehensive strategy, essential for seniors with sclerosis.
Tesia Hardy
October 17, 2025 AT 14:18Just keep at it, you got this!