Imagine taking three different pills every day just to manage your blood pressure, cholesterol, and diabetes. Now imagine one pill that does it all. That’s the power of combination products-and their generic versions are making this easier and cheaper than ever.
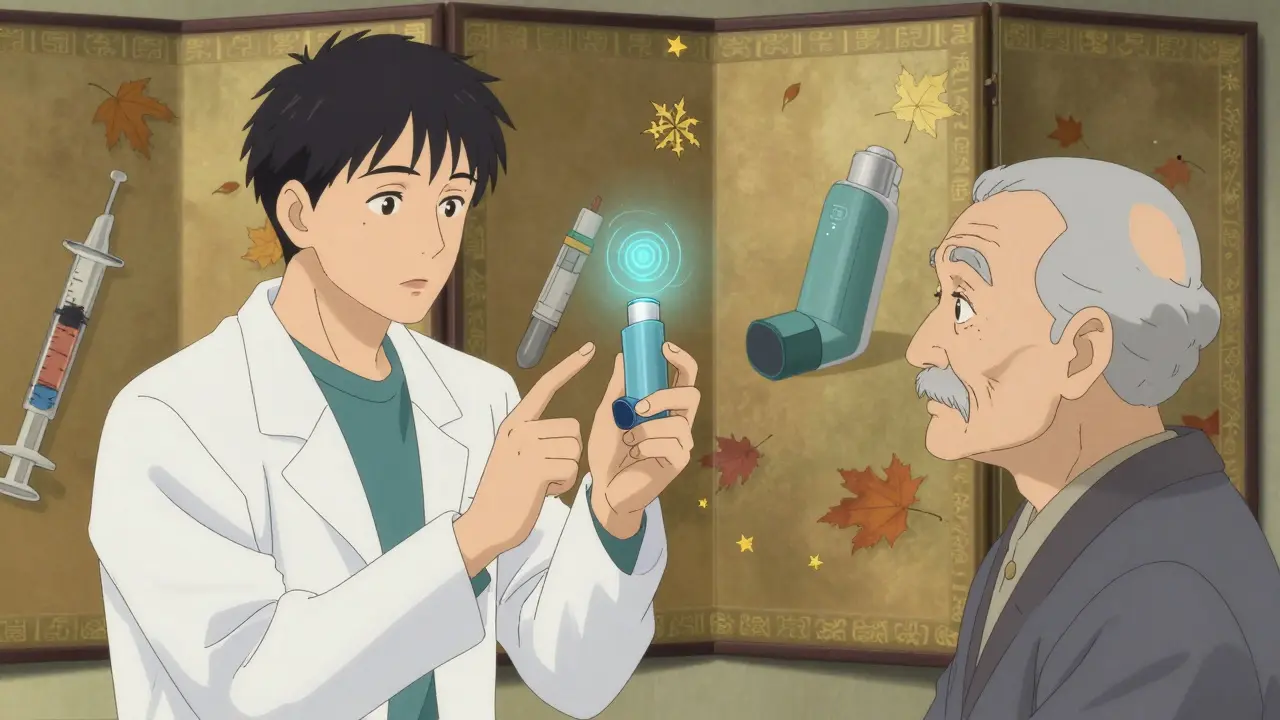
Generic combination products aren’t just cheaper copies. They’re smart, engineered solutions that merge two or more treatments into a single dose or device. Think insulin pens that deliver the right amount without syringes, patches that release medicine slowly through your skin, or inhalers that combine two asthma drugs in one canister. These aren’t sci-fi ideas-they’re everyday tools used by millions. And when they’re generic, they’re saving patients money without sacrificing effectiveness.
How Combination Products Make Treatment Simpler
One of the biggest reasons people stop taking their meds isn’t side effects-it’s complexity. A 2023 study found that adherence drops by 26% when you go from one pill a day to two or more. That’s not a small number. It’s the difference between controlling your condition and ending up in the hospital.
Combination products cut that complexity down. Instead of juggling multiple bottles, timers, and instructions, you get one thing to use. A prefilled insulin pen, for example, removes the guesswork of drawing up doses. No more measuring, no more syringes, no more spills. Patients using these pens report fewer dosing errors-some cut their mistakes from three or four a week to almost none.
Even more advanced options like drug-eluting stents work the same way. These tiny mesh tubes are implanted in blocked arteries and slowly release medicine right where it’s needed. The result? A 30-40% lower chance of the artery clogging again compared to older stents. And now, generic versions of these stents are available, giving the same protection at a fraction of the cost.
Why Generic Versions Work Just as Well
Some people worry that generic means weaker. That’s not true for combination products. The FDA requires generic versions to match the brand-name product in every meaningful way: same active ingredients, same dose, same release timing, and same device performance.
For example, if a brand-name auto-injector needs 8 Newtons of force to activate, the generic must do the same. If a patch delivers 1.0 mg of nicotine per hour, the generic must hit that number within a tight range. The FDA tests these devices under real-world conditions-simulating how patients actually use them. Failure rates must stay below 0.1%. That’s stricter than most consumer electronics.
And it’s not just about the drug. The device matters too. A generic inhaler might look different, but if it delivers the same amount of medicine to the lungs with the same puff technique, it works. Studies show patients on generic combination products have adherence rates 8.7 percentage points higher than those on brand-name versions-likely because they’re more affordable.
The Cost Advantage That Changes Outcomes
Price is the silent killer of adherence. The FDA found that 23.4% of patients skip doses because they can’t afford their meds. That number jumps even higher for chronic conditions requiring daily treatment over years.
Generic combination products typically cost 30-80% less than their brand-name counterparts. A diabetes patient using a branded insulin pen might pay $200 a month. The generic version? $50. That’s not a luxury-it’s survival. And when cost drops, adherence rises. Patients are more likely to refill, more likely to take it as directed, and less likely to end up in the ER.
It’s not just about individual savings. Health systems save too. Fewer hospital visits, fewer complications, fewer emergency procedures. In the U.S., the Inflation Reduction Act is pushing even more generic competition for combination products, with approvals expected to rise 40% between 2024 and 2026.
Where Things Get Tricky: Switching Between Generics
Here’s the catch: not all generics are identical in how they feel or work-even if they’re therapeutically the same.
Take inhalers. Two different generic versions might deliver the same medicine, but one might require a slower inhale, another a sharper one. A COPD patient switching between them without proper training might miss doses, thinking the medicine isn’t working. On patient forums, people report confusion: “I used to puff like this, now I have to do it differently.”
This is where pharmacy substitution becomes a problem. A patient might get one generic in January, another in March, and a third in June-all approved, all legal, all different in feel. Without clear instructions each time, adherence can slip.
Studies show this happens in 32% of cases. It’s not the fault of the drugs-it’s the lack of consistent patient education. When patients are handed a new device with no explanation, they assume it’s broken-or worse, that the medicine doesn’t work.
What Works: Training, Clarity, and Communication
The solution isn’t more regulation-it’s better communication.
Simple training sessions make a huge difference. For a transdermal patch, five minutes of instruction is enough. For an auto-injector? 20-30 minutes of hands-on practice. Visual guides, diagrams, and even QR codes linking to video tutorials help. One study found that patients who received clear instructions were 17-22% more likely to stick with their regimen.
Doctors and pharmacists need to talk about the switch-not just hand over a box. Saying, “This is the same medicine, but the pen works a little differently-let me show you,” changes everything. Patients need to feel confident, not confused.
And it’s working. Patients who start on generics are more likely to keep taking them than those who start on brand-name drugs. Why? Because they’re less expensive and often easier to use. The stigma around generics is fading-especially when people see the results.
The Future Is Integrated and Smarter
The next wave of combination products isn’t just about combining drugs. It’s about combining drugs with technology.
Some new generic inhalers now have built-in sensors that track when you use them and send reminders to your phone. Others include dose counters that sync with apps. These aren’t just fancy gadgets-they’re compliance tools. For elderly patients or those with memory issues, a reminder can mean the difference between control and crisis.
The FDA is updating its guidelines to make sure these smart generics meet the same standards as the rest. And with Medicare now negotiating drug prices, more companies are rushing to bring affordable, high-tech combination products to market.
The goal? No patient should have to choose between affordability and effectiveness. Generic combination products are proving that you don’t have to.
Real Impact, Real Numbers
Let’s put this in perspective:
- Combination products improve adherence by 15-25% compared to multiple separate medications.
- Generic versions cost 30-80% less than brand-name ones.
- Patients on generics have 8.7% higher adherence rates than those on brand-name drugs.
- 78% of users say combination products make them more likely to stick to their treatment plan.
- 62% of doctors prefer combination products for chronic disease management because patients actually take them.
These aren’t theoretical benefits. They’re measurable, repeatable, and life-changing.
For someone managing diabetes, heart disease, or asthma, a generic combination product isn’t just a cost-saving trick. It’s a lifeline. It’s one less thing to forget. One less bottle to carry. One less reason to skip a dose.
And that’s why they’re not just growing-they’re transforming how care is delivered.
Are generic combination products as effective as brand-name ones?
Yes. The FDA requires generic combination products to match the brand-name version in active ingredients, dosage, release timing, and device performance. This includes how much force is needed to activate an injector, the accuracy of a dose, and how the medicine is absorbed. Testing is rigorous-failure rates must be below 0.1%. If it works for the brand, the generic must work the same way.
Why do some patients feel like generic versions don’t work as well?
It’s usually not the medicine-it’s the device. Different generic versions might have slightly different shapes, button placements, or inhalation techniques. A patient who switches from one generic inhaler to another might need retraining. Without clear guidance, they may think the medicine isn’t working, when really, they’re just using it differently. Proper counseling fixes this.
Can I ask my pharmacist to always give me the same generic version?
You can ask, but pharmacies often switch generics based on cost and availability. If consistency matters to you-especially with complex devices like inhalers or auto-injectors-ask your doctor to write "Dispense as Written" or "Brand Necessary" on the prescription. This legally prevents substitution unless you or your doctor approve it.
What types of combination products are most common?
The most common are insulin pens (diabetes), inhalers (asthma/COPD), transdermal patches (pain, nicotine, hormones), and drug-eluting stents (heart disease). These are all designed to simplify dosing and improve adherence. Newer ones include smart pens and inhalers with digital tracking to remind patients when to take their dose.
How do I know if a combination product is right for me?
Talk to your doctor if you’re taking three or more pills a day, missing doses, or struggling with complex delivery systems like syringes or inhalers. Combination products are especially helpful for chronic conditions like high blood pressure, diabetes, asthma, or heart disease. Ask: "Is there a combination version available? Would it be easier for me to use?"

Jessica Salgado
December 17, 2025 AT 04:26Okay but have you seen the packaging on some of these generic inhalers? One minute you’re using a sleek blue one, next week it’s a clunky white thing with a button that feels like it’s gonna snap. No one tells you the puff technique changed. I had to YouTube it. That’s not patient-friendly-it’s a compliance trap.
Josh Potter
December 18, 2025 AT 13:07Bro this is why I love generics. I used to pay $300/month for my combo inhaler. Now I pay $45. Same meds. Same results. I don’t care if the plastic is cheaper-I’m breathing. And I’m not broke. End of story.
Kent Peterson
December 19, 2025 AT 19:47Let’s be real-this whole ‘generic equals equal’ thing is a scam cooked up by Big Pharma and the FDA to push down prices. You think a $50 inhaler has the same valve precision as a $200 one? Please. The FDA tests are a joke. I’ve had two different generics that felt like they were delivering air, not medicine. My lung function dropped. They don’t test real-world wear and tear-only lab conditions.
BETH VON KAUFFMANN
December 20, 2025 AT 15:38It’s not about whether the drug is bioequivalent-it’s about the haptics. The ergonomics. The tactile feedback. A patient doesn’t care about FDA’s 0.1% failure rate-they care if the pen clicks the same way it did last month. When you switch generics and the device feels ‘off,’ your brain assumes the drug isn’t working. That’s cognitive dissonance, not pharmacology. And nobody trains patients on this. It’s systemic negligence.
Donna Packard
December 20, 2025 AT 20:37I just want to say thank you for writing this. My mom’s on a generic combo pill for BP and diabetes-she used to forget half her meds. Now she takes one pill at breakfast and says she feels more in control. No more pill organizers, no more anxiety. It’s small, but it’s huge.
Victoria Rogers
December 22, 2025 AT 14:42And yet-why are we letting generic manufacturers get away with changing the device design every time the contract flips? It’s not ‘affordability,’ it’s exploitation. One month the patch is adhesive A, next month it’s adhesive B-skin irritation spikes. We’re treating patients like lab rats. This isn’t innovation. It’s cost-shifting dressed up as progress.
Patrick A. Ck. Trip
December 24, 2025 AT 01:00I think the real win here is that more people are actually taking their meds now. I work in a clinic. Before generics, we’d see patients every 3 months with worsening numbers. Now? They’re coming in every 6 months with stable labs. The tech-enabled ones? Even better. One guy got a smart insulin pen that texts him when he misses a dose. He said it saved his life. That’s what matters.
Raven C
December 25, 2025 AT 21:20One might argue that the commodification of therapeutic devices-reducing them to interchangeable, cost-optimized artifacts-undermines the very dignity of patient autonomy. The aesthetic, tactile, and ergonomic nuances of medical devices are not trivial; they are constitutive of therapeutic efficacy. To presume equivalence based solely on pharmacokinetic parameters is to commit a category error of monumental proportions.
Naomi Lopez
December 26, 2025 AT 03:33My pharmacist switched my generic stent without telling me. I didn’t even know until I saw the box. Now my arm feels weird when I lift things. I’m not paranoid-I’m informed. And yes, I’m going to ask for the original brand next time. I’m not a guinea pig.